vol. 16 no. 1, March, 2011
vol. 16 no. 1, March, 2011 | ||||
Technology plays an increasingly critical role in current service markets. In this regard, new digital and Internet-related technologies are dramatically modifying how companies, employees, and customers interact in service encounters (Alba et al. 1997; Bitner et al. 2000; Hoffman and Novak 1996; Parasuraman and Colby 2001; Parasuraman and Zinkhan 2002; Zeithaml et al. 2000). In health-care, Internet technologies have the potential to improve the provision of health and patient care services like no other communications medium in the past (Kassirer 2001; Shepherd and Fell 1997). This sector, where encounters between health staff and patients determine to a great extent service quality and patient satisfaction, will require challenging modifications (e.g., changing the behavioural patterns of patients, physicians, and other health staff), in order to fully benefit from the improvements promised by Internet technologies.
The term eHealth is widely used to refer to 'health services and information delivered or enhanced through the Internet and related technologies' (Eysenbach 2001). A recent literature review has identified fifty-one different definitions of eHealth, all showing clear references to health and technology (Oh et al. 2005). The broad scope and interdisciplinary characteristics of eHealth have also been acknowledged. Key elements of this field include the use of networked digital and Internet technologies, especially for communication purposes, and 'its application to all health stakeholder groups' (Pagliari et al. 2005).
The eHealth-related attitudes and behaviour of both physicians' (Brooks and Menachemi 2006; Garritty and El Emam 2006; Murray et al. 2003; Patt et al. 2003; Potts and Wyatt 2002; Sands 1999; Slakey and Nowfar 2004) and patients' (Beckjord et al. 2007; Dutta-Bergman 2004; Hurling et al. 2007; Ross et al. 2005) have been analysed in previous studies. In general, patients have shown a more optimistic view than physicians (Katz et al. 2004; Murray et al. 2003; Ross et al. 2005), with regard to the benefits provided by the use of eHealth services (e.g., patient-physician e-mail communications or patients' Internet health information seeking). Patients' health-related Internet use has focused mainly on searching for health information online (Dutta-Bergman 2004). In the US, recent estimates of citizens' Internet use to seek health information have ranged from 73% to 83% of Internet users (Pew Research Center 2006; Ybarra and Suman 2006). A study carried out in seven European countries has reported similar estimates (71% of Internet users) for European citizens' use of Internet health information (Andreassen et al. 2007).
Patients' use of the Internet for health information has been shown to provide more benefits than problems (Potts and Wyatt 2002; Schwartz et al. 2006). In this regard, most physicians believe that the benefits provided by patients' online health information seeking depend highly on the quality of consulted Internet health information (Murray et al. 2003). Nevertheless, recent results have shown that most patients still verify and discuss Internet health information with their physicians (Schwartz et al. 2006). Therefore, doctors continue to be patients' first option to make an informed medical decision about their medical care (Hart et al. 2004). More active eHealth uses, such as exchanging e-mails with physicians, have shown much lower (though slowly increasing) adoption rates among patients (Beckjord et al. 2007; Murray et al. 2003; Potts and Wyatt 2002).
A large majority (90%) of US physicians (Casebeer et al. 2002), and approximately 70% to 84% of European physicians (European Commission 2008; Manhattan Research 2006), have been reported to access the Internet for various purposes. Physicians use the Internet mostly to search for medical information (Casebeer et al. 2002), in sources such as online journals or literature databases (e.g., Medline) (Flanagan et al. 2003; Manhattan Research 2006). Conversely, physicians are quite sceptical about the potential benefits provided by patient-physician e-mail communication (Brooks and Menachemi 2006; Casebeer et al. 2002). Less than 25% of US and European physicians have been reported to exchange e-mails with their patients (Manhattan Research 2006; Slakey and Nowfar 2004). Perceived benefits include easier chronic-disease management (Slakey and Nowfar 2004) and increased flexibility in responding to patients' requests (Patt et al. 2003). Perceived risks include concerns about the effective integration of patient e-mail into daily workflow, confidentiality issues, lack of time, and reimbursement for provided patient care communication (Curry 2007; Miller et al. 2004; Patt et al. 2003).
Electronic health-care records, also known as electronic medical, health, or patient records, represent integrated information systems which electronically record and store individual administrative and medical patient information (Audet et al. 2004; Burt and Sisk 2005; Curry 2007; Fundación Telefónica 2006), providing physicians, pharmacists, and patients with a 'one-stop access to medication history, prescriptions, lab test results, health claims information, allergies, diagnoses, and so forth' (Curry 2007: 129 ). These systems have been argued to be a 'central component of health information technology' (Curry 2007: 129) and to contribute to increased efficiency of physicians' professional activities (Flanagan et al. 2003).
In the US, estimates for physicians' adoption of electronic health-care records have ranged between 13% and 27% in private medical practices (Audet et al. 2004; Burt and Sisk 2005; Hillestad et al. 2005; Miller and Sim 2004), and between 20% and 25% in hospital settings (Hillestad et al. 2005). Higher estimates between 65% and 85% have been reported for European physicians (Manhattan Research 2006; European Commission 2008). A recent pan-European survey confirms that the use of electronic medical records is very widespread among general practitioners in the European Union, both for digital storage of administrative (84% of physicians) and medical (85%) patient-identifiable data (European Commission 2008). It is worth noting that nearly all general practitioners in the United Kingdom currently use electronic health-care record systems in their medical practices: between 95% and 100% of UK physicians have been shown to electronically store administrative and medical patient data (European Commission 2008; Fundación Telefónica 2006; Schade et al. 2006).
The adoption of other eHealth services and technologies has been uneven. Higher adoption rates (59%) have been seen for physicians' computerised access to laboratory results (Audet et al. 2004). Adoption estimates of handheld mobile devices or PDAs have ranged from 45% to 85% for US physicians (Garritty and El Emam 2006) and one third of European physicians (Manhattan Research 2006). However, physicians' widespread use of online prescribing services has faced numerous problems (Grossman et al. 2007; Smith 2006), with reported usage estimated at 27% among US physicians (Audet et al. 2004).
Previous research has also shown significant differences, both at the national and regional level, with regard to the development and adoption of Internet-related technologies in diverse sectors (Guillén 2002; Ngini et al. 2002). These differences are even observable among developed countries in the European Union (Fundación Telefónica 2006). In this regard, individuals from Northern European countries show higher rates of Internet adoption, as well as far more developed digital infrastructures (Crosby and Johnson 2002). The unequal access to Internet technologies and slower Internet adoption processes in technologically less advanced countries (the digital divide) limit the potential positive effects of Internet technologies on the provision of health services in such regions.
Diverse studies have also dealt with the influence of other external variables (e.g., sex and age) on citizens' and patients' Internet use (Korgaonkar and Wolin 1999; Schwartz et al. 2006), as well as physicians' professional use of eHealth services (Burt and Sisk 2005). Patients' Internet access and online searches of health information have shown significant associations with age, sex, race, education, and income (Pew Research Center 2006; Schwartz et al. 2006). According to previous studies, men (compared to women) and older patients (especially those aged 65 and over) are less likely to search for health information on the Internet (Korgaonkar and Wolin 1999; Pew Research Center 2006; Schwartz et al. 2006). Additionally, white patients (compared to African American individuals), with college education (compared to less-educated individuals), and higher income (compared to citizens at lower income levels) have shown significantly higher rates of Internet access and use of the Internet to seek health information (Pew Research Center 2006; Schwartz et al. 2006).
Physicians' eHealth use has shown significant relationships with variables like size of the medical practice, age, medical specialty, or geographic location (Audet et al. 2004; Brooks and Menachemi 2006; Burt and Sisk 2005; Garritty and El Emam 2006). Higher usage rates of eHealth services have been observed in larger medical practices, i.e., practices with more physicians (compared to single-physician or small practices) (Audet et al. 2004; Brooks and Menachemi 2006; Burt and Sisk 2005; European Commission 2008; Garritty and El Emam 2006), especially those located in urban zones (compared to rural settings) (Brooks and Menachemi 2006). With regard to physicians' individual traits (age and medical specialty), previous research has shown declines in eHealth use with physicians' age (lower use among older physicians, especially practitioners aged 65 years and above, compared to younger individuals) (Audet et al. 2004; Brooks and Menachemi 2006; Garritty and El Emam 2006), whereas physicians from family medicine or a surgical specialty (compared to other medical specialties) are more likely to use eHealth services (Brooks and Menachemi 2006).
Nevertheless, previous research has also suggested that the influence of specific external indicators (e.g., age) on eHealth use differs across specific eHealth services (Burt and Sisk 2005) or that such indicators may become less relevant in explaining technology use over time (Korgaonkar and Wolin 1999; Rogers 2003). It has been argued that the demographic differences between adopters and non-adopters become less significant as media and technologies mature (Rogers 2003). eHealth services are still in the early stages of diffusion, and so it could be reasonably expected that as different eHealth services become more widespread, there will be less demographic differences between users and non-users (Korgaonkar and Wolin 1999).
The review of previous studies evidences that further research is needed, especially empirical studies into the antecedents, current behaviour, main purposes, and consequences of Internet usage for health purposes. The results of such studies should be taken into account by European, national, and regional authorities, in order to develop suitable promotion strategies, aimed at further integrating new information technologies into patient care services. Such public or private Internet promotion policies should be adapted to specific segments with differing eHealth-related attitudes and behaviour (Miller et al. 2004).
To effectively promote the use of Internet technologies for the provision of patient care services, it is important to understand the nature of physicians' professional uses of the Internet. Thus, this paper aims to clarify (1) the usage patterns of the public Internet and dedicated networks by European general practitioners, and (2) how external factors affect the degree of physicians' usage of eHealth services.
First, European general practitioners are segmented based on their adoption and professional uses of the Internet and general practitioners' networks. These analyses will clarify the existence and behavioural characteristics of different groups of European physicians (i.e., more vs. less advanced eHealth users). Usage indicators of the main eHealth services have been selected for the characterization of segments.
Secondly, the effects of external variables (i.e., country, sex, age, location, and size of the medical practice) on the previously identified groups of eHealth users will be examined. Owing to existing national and regional differences in Internet adoption, these segments are expected to be differently distributed between European countries (Fundación Telefónica 2006). Accordingly, because of strong effects observed in previous studies, age is expected to show a significant decreasing association with physicians' eHealth use (Audet et al. 2004; Garritty and El Emam 2006). The other covariates included in the study (sex, location, and size of the medical practice) are expected to provide less stable and weaker effects on the identified segments of eHealth users (Burt and Sisk 2005; Korgaonkar and Wolin 1999; Rogers 2003).
The empirical analyses are performed on the survey data included in the cross-national dataset 'Flash-Eurobarometer No 126 General Practitioners and the Internet. Flash Eurobarometers are conducted at the request of the European Commission to address special topics and to focus on specific target groups. In this sense, the Flash-Eurobarometer No 126 includes data related to European physicians' use of diverse eHealth services.
The fieldwork was carried out by the national institutes associated with EOS Gallup Europe. Telephone interviews were carried out in all member states of the European Union, using systematic sampling with a constant interval (Statistics Canada 2009), in order to guarantee the representativeness of each national sample for its universe.. In each country, surveyed physicians were selected from the published lists of general practitioners. Interviews were conducted between May 27th and June 19th, 2002.
A total of 3,512 general practitioners participated in the study (approximately 200 from each country). The survey included several questions related to the use of diverse eHealth services and additional socio-demographic indicators (country, age, sex, location, and size of the medical practice) were also employed.
Access to the cross-national database used in this study was provided by the Central Archive for Empirical Social Research (University of Cologne, Germany). This institution offers information on, and online access to, surveys of the Standard and Flash-Eurobarometer series. In general, Flash-Eurobarometer data are free for secondary analyses one year after the fieldwork date.
Several segmentation approaches can be applied to group physicians sharing certain characteristics associated with eHealth use. Researchers from the segmentation field illustrate the usefulness of behavioural profiling of users and consumers, which enables the identification of user categories such as current users, non-users, light users, or heavy users (Ram and Jung 1990; Weinstein 2004). The purposes and frequency of product use (e.g., technology usage) are the principal dimensions used for behavioural segmentation (Weinstein 2004).
In recent research, behavioural segmentation has proved useful in uncovering heterogeneous segments of current Internet users who differ in their online behaviour. Applying behavioural-benefit segmentation, Bhatnagar and Ghose (2004) identified three segments of online shoppers, according to individuals' purchase behaviour in several product categories. More recently, a behavioural-usage segmentation analysis of European citizens yielded five different segments based on the purposes and frequency of their Internet use (Ortega et al. 2007). In line with these studies, a behavioural segmentation approach has been selected to classify European general practitioners, according to their usage patterns of diverse eHealth services. Variables reflecting different degrees of innovativeness in physicians' eHealth-related behaviour are included in the segmentation analyses, which will enable differentiation between more and less innovative groups of general practitioners.
Other available segmentation approaches include the segmentation of customers or users based on geographic variables (e.g.., country or type of locality), demographics (e.g., sex, age or occupation), and psychographic variables (e.g., lifestyles, values, or attitudes) (Weinstein 2004). These alternative segmentation bases are increasingly being applied in online research settings (e.g., Muthitacharoen et al. 2006). For example, a lifestyle segmentation analysis of Internet consumers identified four segments of online shoppers and four segments of online non-shoppers (Swinyard and Smith 2003).
Latent class cluster analysis was selected, to identify homogeneous segments of eHealth adopters among European physicians. Cluster analysis seeks to identify homogeneous subgroups of cases (e.g., individuals) in a population, where the optimal number of groups, the properties of the segments, and group membership are unknown in advance (Garson 2009; Kaufman and Rousseeuw 1990; Vermunt and Magidson 2002). Standard approaches to cluster analysis include the kierarchical, K-means and two-step clustering procedures (Garson 2009). Other methods, such as Q-mode factor analysis, multidimensional scaling, or latent class analysis, offer alternative approaches to cluster analysis (Garson 2009).
Latent class analysis provides a probabilistic model-based clustering approach, which overcomes some of the barriers involved in traditional clustering techniques, such as the normality assumption or the need for equal variances in each cluster (Magidson and Vermunt 2002). Unlike other clustering approaches, such as K-means, the latent class methodology provides formal statistical procedures for determining the number of clusters, eliminates the need to standardise variables prior to cluster analysis and enables the use of variables with mixed scale types (Vermunt and Magidson 2002).
In particular, latent class clustering is especially useful for dealing with categorical variables, which is the case in this study (Vermunt and Magidson 2002). A traditional latent class model is obtained when all indicators are categorical, whereas 'K-Means clustering is limited to interval scale quantitative variables' (Magidson and Vermunt 2002: 41). Therefore, latent class models provide a very flexible methodology to analyse 'continuous, categorical (nominal or ordinal), counts, or any combination of these data' (Vermunt and Magidson 2002: 94). The Bayesian information criterion was selected for the identification of the optimal number of segments. According to Biernacki and Govaert (1999), in clustering contexts this criterion out-performs other classification criteria.
The relative distribution of the identified segments with regard to several external or exogenous variables (i.e., country, sex, age, location, and size of the medical practice) has also been examined (Vermunt and Magidson 2002). For instance, the analyses performed in the present study should clarify whether the relative number of general practitioners, who are classified into more versus less advanced eHealth usage segments, are differently distributed across European countries or age groups. Before describing differences in the distribution of segments based on covariates, researchers should report the results of significance tests (e.g., Χ2 or Wald tests) and measures of the strength of association between the covariates and the identified segments.
In large samples, relationships can be found significant even when the association of variables is very weak. In these cases, measures such as Phi, Cramer's V, or the Contingency Coefficient should be reported in order to fully represent the real strength or intensity of the association between the segments and the covariates. Phi, Cramer's V, and the Contingency Coefficient measure the strength of the relationship between two nominal variables in a contingency table, with values between 0 (no relationship) and 1 (perfect relationship) (Garson 2009b). Phi should be used in 2x2 tables, while Cramer's V or the Contingency Coefficient should be reported when at least one of the variables has more than two categories (Garson 2009b).The evaluation of such indices will clarify the statistical significance of observed differences, that is, the statistical relevance of each exogenous variable or covariate to predict segment membership (Vermunt and Magidson 2002).
From a total sample of 3,512 participants, the authors selected general practitioners who use Internet-enabling devices in their private practices (e.g., personal computers, laptops, or PDAs) for inclusion in subsequent statistical analyses. In most doctors' private offices (2,862 or 81.5%) computer equipment is available. With regard to Internet use in the medical practice, a total of 2,264 professionals (64.5%) were accessing the Internet or a general practitioners' network from their private practices, compared to 96% of health professionals using Internet technologies in the United States (Von Knoop 2003). Only these 2,264 physicians accessing the Internet were included in cluster analysis.
Taking into account the changes in the Bayesian information criterion between the different cluster solutions (see Table 1), three is the optimal number of segments among European general practitioners using the Internet or a general practitioners' network. The classification error for the three-cluster solution is 2.36%.
| Number of clusters | BIC (based on LL) | Change in BIC † |
|---|---|---|
| 1 cluster | 88,102.2 | - |
| 2 clusters | 66,998.0 | -21104.2 |
| 3 clusters (optimal solution) | 63,759.8 | -3,238.2 |
| 4 clusters | 62,152.2 | -1,607.5 |
| 5 clusters | 61,143.8 | -1,008.5 |
| 6 clusters | 60,579.1 | -564.7 |
| † Changes refer to the previous number of clusters in the table | ||
After adding the group of physicians not using the Internet, European physicians can be classified into four segments, according to their professional use of the Internet or a general practitioners' network. These four segments comprise the identified three clusters of eHealth users plus the group of non-Internet users. According to their internal characteristics (described in the following section), the four final segments have been labelled as information searchers, advanced users, laggards, and non-Internet users.
Next, a behavioural characterization of segments is provided, based on the eHealth indicators used to identify the different groups of European general practitioners. To clarify how the identified clusters relate to eHealth nominal variables, Table 2 shows the proportion of physicians (absolute numbers and percentages) (Vermunt and Magidson 2002) using the different eHealth services in each of the eHealth user segments:
| eHealth indicators | Information searchers | Advanced users | Laggards | Non-Internet users |
|---|---|---|---|---|
| Accessing medical Web sites | 834 (82.7%) | 494 (67.1%) | 106 (20.4%) | 0 (0%) |
| Searching for prescribing information | 731 (72.5%) | 453 (61.5%) | 92 (18%) | 0 (0%) |
| Accessing information for continuing education | 980 (97.2%) | 536 (72.8%) | 128 (24.6%) | 0 (0%) |
| Exchanging views with other doctors | 348 (34.5%) | 305 (41.4%) | 49 (9%) | 0 (0%) |
| Consulting medical journals | 844 (83.7%) | 453 (61.5%) | 97 (18.7%) | 0 (0%) |
| Transferring patient identifiable data | 0 (0%) | 736 (100%) | 0 (0%) | 0 (0%) |
| Patient data transfers: submitting patient care reimbursement claims | 0 (0%) | 296 (40.2%) | 0 (0%) | 0 (0%) |
| Patient data transfers: transferring administrative patient data to a secondary care provider | 0 (0%) | 307 (41.7%) | 0 (0%) | 0 (0%) |
| Patient data transfers: transferring patient medical data to other medical care | 0 (0%) | 362 (49.2%) | 0 (0%) | 0 (0%) |
| Patient data transfers: receiving results from laboratory analyses and other diagnostic procedures | 0 (0%) | 567 (77%) | 0 (0%) | 0 (0%) |
| Patient data transfers: exchanging e-mails with patients | 0 (0%) | 230 (31.3%) | 0 (0%) | 0 (0%) |
| Patient data transfers: offering telemedicine services to patients | 0 (0%) | 69 (9.4%) | 0 (0%) | 0 (0%) |
| Patient data transfers: electronic prescribing | 0 (0%) | 268 (36.4%) | 0 (0%) | 0 (0%) |
| Patient data transfers: written consent obtained for transferring patient data | 0 (0%) | 120 (16.3%) | 0 (0%) | 0 (0%) |
| Patient data transfers: oral consent obtained for transferring patient data | 0 (0%) | 220 (29.9%) | 0 (0%) | 0 (0%) |
| Patient data transfers: no specific consent obtained for transferring patient data | 0 (0%) | 325 (44.2%) | 0 (0%) | 0 (0%) |
| Patient data transfers: always use electronic signatures in communicating patient medical data | 0 (0%) | 94 (12.8%) | 0 (0%) | 0 (0%) |
| Patient data transfers: sometimes use electronic signatures in communicating patient medical data | 0 (0%) | 74 (10.1%) | 0 (0%) | 0 (0%) |
| Patient data transfers: no use of electronic signatures in communicating patient medical data | 0 (0%) | 527 (71.6%) | 0 (0%) | 0 (0%) |
| Electronic health-care record provided by national or regional health authority | 149 (14.8%) | 112 (15.2%) | 95 (18%) | 0 (0%) |
| Electronic health-care record purchased specifically for the practice | 534 (53%) | 424 (57.6%) | 134 (25.8%) | 0 (0%) |
| No use of electronic health-care records | 309 (30.7%) | 182 (24.7%) | 257 (49.4%) | 0 (0%) |
| Website with administrative information only | 172 (17.1%) | 128 (17.4%) | 60 (11.5%) | 0 (0%) |
| Website with administrative plus health information | 138 (13.7%) | 109 (14.8%) | 31 (6%) | 0 (0%) |
| Website with interactive patient appointment scheduling | 27 (26.8%) | 30 (4%) | 5 (1%) | 0 (0%) |
| No Website for the medical practice | 697 (69.1%) | 496 (67.4%) | 405 (77.9%) | 0 (0%) |
Segment 1: Information searchers (n=1008; 28.7%)
The use of Internet-based networks to search for health-related information is the main characteristic of this segment. Out of the 1,008 physicians classified as information searchers 980 (97.2%) were accessing information online for the purpose of continuing education. A majority of these doctors also reported consulting medical journals (844; 83.7%), accessing medical associations' Websites for professional-oriented information (834; 82.7%), and searching for prescribing information (731; 72.5%).
These doctors do not transfer patient identifiable data through the Internet or a general practitioners' network. Information searchers show a moderate use of electronic health-care records, which are specifically purchased for the medical practice (534; 53%). A high proportion of physicians in this group did not report using Websites for their practices (697; 69.1%).
Segment 2: Advanced users (n=736; 21%)
Like Information searchers, general practitioners in this group are searching for health information for professional purposes on the Internet. The key distinguishing characteristic of this segment relates to the use of the Internet-based networks for transferring patient identifiable data (736; 100%). Practically all members of this segment send or receive this kind of patient data online. The main purposes of these data transfers include: receiving results from laboratories and other diagnostic procedures (567; 77%); submitting patient care reimbursement claims (296; 40.2%); transferring patient medical data to other medical care providers for the purposes of continuity of care (362; 49.2%); and transferring administrative patient data to a secondary care provider (307; 41.7%).
E-mail communication with patients was not yet a widespread activity (230; 31.3%). These 230 general practitioners represented 6.5% of the 3,512 physicians who participated in this study. Internet technologies were rarely used to offer telemedicine (69; 9.4%) or electronic prescribing services to patients (238; 36.4%). A high proportion of physicians transferring patient data did not obtain specific patients' consent (325; 44.2%). The majority of such physicians do not use electronic signatures in communicating patient medical data online (527; 71.6%). The use of electronic health-care records was moderate among advanced users. Again, most of these systems were specifically purchased for the medical practice (424; 57.6%).
Segment 3: Laggards (n=520; 14.8%)
This segment showed a less sophisticated use of Internet-based networks for professional purposes in all analysed areas. These physicians reported a limited use of the Internet or dedicated general practitioners' networks for purposes related to medical information searches, such as accessing medical Websites (106; 20.4% of physicians in this group) or seeking information for continuing education (128; 24.6%). Laggards do not transfer patient identifiable data through the Internet or a general practitioners' network. They rely less frequently on electronic health-care records, as only 134 out of 520 doctors classified as Laggards (12.3%) reported having purchased one of these systems. Web sites were rarely used to manage the private medical practices, either to provide only administrative information (60; 11.5%) or administrative and health information (31; 6%).
Segment 4: Non-Internet users (n=1248; 35.5%)
It is important to emphasise the high proportion of European health professionals who were not taking advantage of the new possibilities afforded by Internet technologies for the provision of health-care services. These physicians reported not accessing the Internet or a dedicated general practitioners' network and, consequently, were not asked about their eHealth-related behaviour. Therefore, the identification of the group of non-Internet users was not a result of the latent class cluster analyses. It was added as an additional group or segment, which included all European general practitioners not using any kind of eHealth services.
An attempt has been made to characterize the identified segments, according to several external variables. These analyses should contribute to the debate on whether geographic criteria, demographic traits, or job characteristics show significant effects on the acceptance and use of Internet technologies and other technological innovations.
One of the main purposes of this study relates to the examination of potential national differences, related to European physicians' use of the Internet or a general practitioners' network. For this purpose, the latent class analyses provide a first way to test the statistical significance of the association between the covariates and the identified segments: the Wald test. As a statistical or significance test (Polit 1996), the Wald test will be used to evaluate whether a statistically significant association exists (or not) between the analysed exogenous variables (e.g., country) and the identified segments of eHealth users.
Based on the results of the Wald test, provided by the performed latent class cluster analysis, the effects of the country variable on the identified groups of Internet users is very significant (Wald=467.5; P<.001), which suggests the existence of significant national differences among European countries (Fundación Telefónica 2006).
Whether the four identified segments, including the non-Internet users group, show statistical significant differences between countries was also investigated. The relative distribution of the identified segments in the analysed countries has been displayed in a contingency table. Again, the results of a significance test, such as the Χ2 test (Χ2=1516; P<.001), suggest the existence of significant differences among countries.
Because of the large sample size in this study (3,512), the authors also provide measures of the association between the segments and the covariates. For the country covariate, the analysis of a 15x4 contingency table (larger than 2x2) recommends the selection of Cramer's V and the Contingency Coefficient, instead of Phi (suitable for 2x2 tables) (Garson 2009b), to evaluate the strength of association between country and segment membership. In this case, the values of Cramer's V (0.38) and the Contingency Coefficient (0.55) confirm the existence of strong influences (Garson 2009b) of physicians' country on the probability to be classified into more vs. less advanced eHealth user segments (Vermunt and Magidson 2002).
The following national trends in the use of the Internet and dedicated healthcare networks among European general practitioners can be observed (see Table 3 and Figure 1):
| Country | Information searchers | Advanced users | Laggards | Non-Internet users |
|---|---|---|---|---|
| Belgium | 30 (15%) | 60 (30%) | 10 (5%) | 100 (50%) |
| Denmark | 21 (11%) | 152 (76%) | 6 (3%) | 21 (10%) |
| Germany | 80 (26%) | 17 (6%) | 29 (10%) | 174 (58%) |
| Greece | 30 (15%) | 8 (4%) | 10 (5%) | 152 (76%) |
| Spain | 93 (25%) | 53 (14%) | 30 (8%) | 194 (53%) |
| France | 96 (24%) | 60 (15%) | 148 (37%) | 96 (24%) |
| Ireland | 67 (33%) | 14 (7%) | 33 (17%) | 86 (43%) |
| Italy | 119 (39%) | 48 (16%) | 29 (10%) | 105 (35%) |
| Luxembourg | 29 (36%) | 4 (5%) | 11 (13%) | 37 (46%) |
| Holland | 22 (11%) | 90 (44%) | 34 (17%) | 56 (28%) |
| Austria | 41 (20%) | 61 (30%) | 13 (7%) | 85 (43%) |
| Portugal | 43 (21%) | 16 (8%) | 21 (11%) | 120 (60%) |
| Finland | 101 (67%) | 15 (10%) | 25 (17%) | 9 (6%) |
| Sweden | 62 (31%) | 55 (27%) | 78 (39%) | 5 (3%) |
| UK | 178 (58%) | 83 (27%) | 39 (12%) | 8 (3%) |
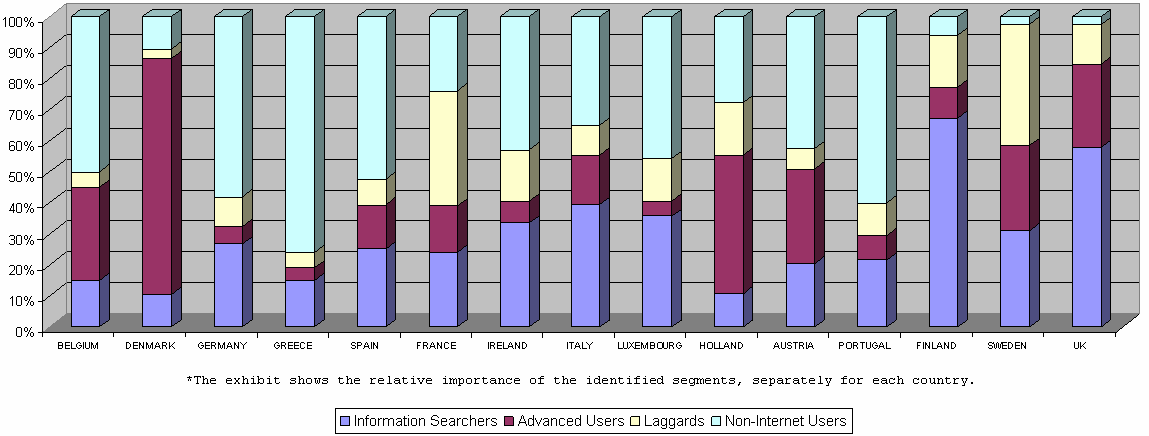
Laggard countries. The number of non-Internet users is very high in these countries; relatively few advanced users and information searchers can be found: Greece, Spain, Germany, and Portugal.
Follower countries. The number of advanced users and information searchers is moderate, but the number of non-Internet users is still quite high: Belgium, France, Ireland, Italy, Luxembourg, Holland, and Austria.
Advanced countries. These countries are characterized by very few non-Internet users. There is a high number of advanced users and information searchers: Sweden, the United Kingdom, Finland, and Denmark. Denmark stands out as the country with the highest number of advanced users.
While country differences in the adoption of eHealth services resemble, to a great extent, traditional economical and infrastructural differences between European countries, attitudinal, perceptual, or cultural factors also exert significant influences on the acceptance of Internet technologies for health professional purposes. Further research should examine the role and relative importance of physicians' individual characteristics in the adoption of eHealth services.
Based on the results of the latent class analysis, the effects of sex on the identified groups of Internet users are significant (Wald=17.9; P<0.001). The tests of sex differences between the four segments provided the following results (Χ2=17.8; P<0.001; Cramer's V=0.071; Contingency Coefficient=0.071). As suggested by these measures, there is a very weak association between sex of surveyed physicians and their classification in each of the identified segments.
These results show very similar profiles for men and women with regard to the classification of physicians in the different segments. Although the distribution patterns of the identified clusters among men and women are very similar, it can be observed that male physicians show a slightly more sophisticated use of Internet technologies for their medical practice. A higher percentage of women is included in the laggards group (165; 18.4%), compared to 13.2% of men (345).
As a conclusion, these results confirm previous research, suggesting that sex is becoming less significant in explaining technology usage, especially in highly educated groups, like physicians (Burt and Sisk 2005).
This study has also examined if there are significant age differences in physicians' adoption of Internet-related technologies for professional purposes. According to the results of the cluster analysis, the effect of age on the identified classes of Internet users is statistically significant (Wald=39.8; P<0.001). Further analysis of age differences between the four segments showed the following results: Χ2=255.3; P<0.001; Cramer's V=0.16; Contingency Coefficient=0.26. These measures indicate a moderate association between physicians' age and their classification in one of the identified segments.
Next, a more detailed analysis of age differences is provided based on the relative distribution of eHealth user segments among different age groups (see Table 4 and Figure 2):
| Age | Information searchers | Advanced users | Laggards | Non-Internet users |
|---|---|---|---|---|
| <35 | 62 (32%) | 45 (23%) | 40 (20%) | 48 (25%) |
| 36-40 | 135 (35%) | 85 (22%) | 59 (15%) | 107 (28%) |
| 41-45 | 266 (34%) | 163 (21%) | 100 (13%) | 244 (32%) |
| 46-50 | 272 (33%) | 174 (21%) | 132 (16%) | 254 (30%) |
| 51-55 | 164 (26%) | 150 (24%) | 97 (16%) | 201 (34%) |
| 56-60 | 74 (23%) | 80 (25%) | 47 (14%) | 124 (38%) |
| 61-65 | 20 (14%) | 19 (14%) | 16 (11%) | 87 (61%) |
| >66 | 14 (7%) | 12 (6%) | 16 (9%) | 148 (78%) |
| DK / NA | 11 (19%) | 8 (14%) | 3 (5%) | 35 (62%) |
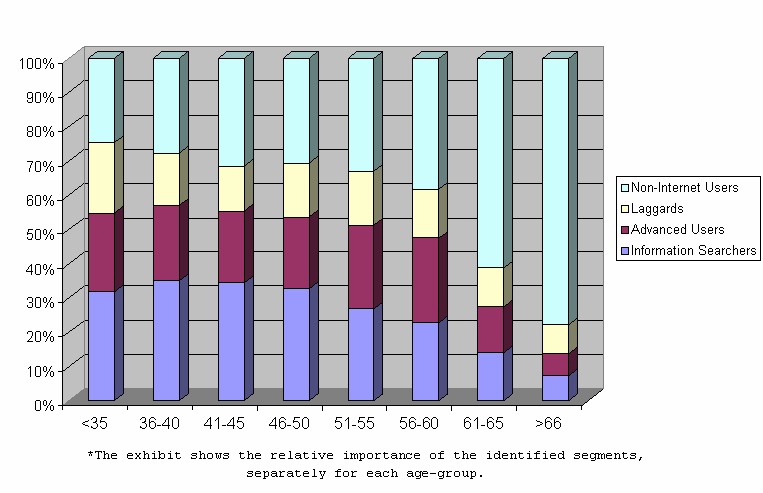
Younger physicians (less than 35 years old) show the highest percentage of Internet users. Physicians aged between 36 and 40 years present the most sophisticated use of eHealth technologies (highest number of advanced users and Information searchers). In general, physicians under 60 years show quite similar uses of Internet technologies, with only slight differences observed among physicians aged between 50 and 60 years: fewer Information searchers and a higher share of non-Internet users, compared to younger physicians.
Behavioural differences are most noticeable between physicians over 60 years and those in the lower age groups. Comparatively, a clear reduction in Internet use is observable among older physicians (over 60 years old). In this sense, the respective shares of non-Internet users among general practitioners in the 61-65 and >66 age groups are 61% (87) and 78% (148), compared to percentages of non-users between 25% and 38% among younger physicians. Physicians aged 60 or more also report a very limited use of the different eHealth services. This trend is clearly reflected in lower percentages (6% to 14%) of eHealth users (Advanced users, Information searchers, and Laggards) among older physicians.
Thus, the results point to a clear decline in the use of the Internet or a general practitioners network for physicians in ages over 60 years. These results are consistent with several recent investigations showing the existence of significantly lower usage rates of eHealth services among physicians (e.g., general practitioners) aged 65 years and above, compared to younger individuals (Audet et al. 2004; Brooks and Menachemi 2006; Garritty and El Emam 2006). However, caution must be taken in attributing the observed age differences to a real 'age effect', resulting from a life-cycle orientation of individuals' technology-related needs and preferences (Morris and Venkatesh 2000).
Owing to the similarity of eHealth usage behaviour between young and middle-aged physicians (practitioners aged 60 or below), the observed differences between older (over 60 years old) and younger general practitioners suggest the existence of a cohort effect rather than an age effect, because of physicians being born, educated, and trained at different time points relative to the development and adoption of personal computers and the Internet. Young and middle-aged physicians are more likely to have been exposed to technology (e.g., information technology) in their private lives and professional careers. The relatively recent introduction of eHealth services in the European market suggests that a digital divide among older (over 60 years) and younger physicians could be regarded as a transitory situation.
The Wald statistic and the z-values for the external variable location of practice indicate that this covariate does not exert a statistically significant effect on the identified segments of Internet users (Wald=1.87; P=.76). Further tests confirm the existence of very homogeneous usage patterns of technological healthcare networks for physicians working in different settings, whether metropolitan zones, other town, or rural areas (Χ2=24.7; P=.03; Cramer's V=0.048; Contingency Coefficient=0.084).
Although not statistically significant, it is worth noting that general practitioners working in rural settings show more sophisticated usage patterns of eHealth technologies than physicians in metropolitan zones, with a higher share of advanced users and Information searchers. Thus, possible concerns about the existence and widening of a digital divide between metropolitan and rural areas (Brodie et al. 2000; Brooks and Menachemi 2006) have not been confirmed for European health practitioners.
The cluster analysis indicates that the effect of size of practice on the identified groups of Internet users is not statistically significant (Wald=6.4; P=0.38). After the inclusion of the non-Internet users group, further tests suggest the existence of a statistically significant relationship between this covariate and the identified segments (Χ2=326.7; P<0.001; Cramer's V=0.18; Contingency Coefficient=0.29). The value of Cramer's V points to a weak increasing relationship between size of the medical practice and the usage rates of Internet-based healthcare networks. This association should be interpreted with caution, as the results of the latent class cluster analysis were not statistically significant.
This research has identified four segments of European physicians, based on their actual uses of eHealth services: information searchers, advanced users, laggards, and non-Internet users. The proposed classification of European physicians into more or less advanced or innovative segments of eHealth users is consistent with the most-widely known categorizations of technology users and consumers (e.g., Parasuraman and Colby 2001; Rogers 2003). Five categories of technology adopters were proposed by Rogers (2003), based on the time needed for the adoption of technological innovations by different individuals. Different citizen and consumer groups (generally four or five) have also been identified in previous research (Parasuraman and Colby 2001; Tsikriktsis 2004) according to people's level of technology readiness (i.e., general attitude towards technology).
However, unlike Rogers's (2003) analysis of technology adoption over time, the present study identifies segments by examining the innovativeness of physicians' eHealth usage in a cross-sectional research. Additionally, the application of different criteria for the identification of segments (eHealth usage data) limits the possibilities to draw comparisons between the aforementioned technology-related taxonomies and this study. A more direct link can be established between the four identified segments of general practitioners, based on their eHealth usage patterns, and usual categorizations in behavioural-usage segmentation studies which range from non-usage to intensive or advanced usage profiles (Ram and Jung 1990; Weinstein 2004).
The identification of these segments should provide a valuable basis for the development of suitable Internet promotion strategies, adapted to the needs of the different groups. Strategies targeted at the laggards and non-Internet users should focus on explaining the benefits provided by Internet technologies in general, not only for health purposes. Training should be offered to these groups, where the needed skills for Internet use can be acquired. Later, these people should be offered continuous education on the possibilities afforded by Internet technologies for their professional activities. These courses should emphasise the potential benefits of Internet technologies in terms of efficiency and improved patient satisfaction.
However, the limited use of information technology among the laggards and non-Internet users should not only be attributed to low perceptions of usefulness or behavioural control. Lower adoption rates of eHealth services may reflect other concerns and perceived risks among physicians, related to the real benefits provided by direct patient-physician e-mail communication, including: lack of clear empirical support for the contributions of eHealth to improvements in the quality of health-care; concerns about the integrity of electronically stored and transmitted patient data; or the effects of Internet health information on patients' health, which are highly dependent on the quality of information (Brooks and Menachemi 2006; Casebeer et al. 2002; Curry 2007; Suh and Han 2003; Yarbrough and Smith 2007). Such legitimate concerns and risks should be adequately assessed and clarified to ensure an effective promotion of the Internet and eHealth services in the lower-use groups. Addressing physicians' perceived concerns and risks should also help to prevent potential adverse and undesired outcomes caused by the implementation of eHealth systems (especially those harming patients' health).
Policies targeted at Information searchers should focus on explaining the potential benefits (e.g., time and efficiency improvements) of using the Internet or a dedicated healthcare network to transfer patient identifiable data. Additionally, potential confidentiality and privacy problems in transferring administrative and medical patient data need to be specifically considered and clarified in training and marketing programs aimed at this segment. Previous studies have stressed the importance of physicians' privacy and security-related concerns, mainly with regard to the security, confidentiality, and integrity of digitally stored and transmitted patient identifiable data (Dixon 2007; Suh and Han 2003; Yarbrough and Smith 2007). Privacy and security problems in electronic health transactions and communications may pose significant risks to patient diagnostic and therapeutic processes, e.g., medical errors (Dixon 2007; Kassirer 2001; Murray et al. 2003).
Both Information searchers and advanced users should receive training on how e-mail patient communication, electronic prescribing, and Websites can help them to improve the management of their professional practices, as these are not widespread activities yet. In addition to the previously detailed influencing factors, differences in the national health-care systems of European countries may help to explain why certain eHealth services such as electronic prescribing or patient-physician e-mail communication are not widely adopted in more advanced segments (Information searchers and Advanced users), and the extent to which health-care procedures and management can be actually improved by use of the Internet and eHealth services.
Advanced users' main characteristic relates to the use of Internet technologies for transfers of patient identifiable data. Nonetheless, the protection of patients' privacy, such as obtaining patients' consent or the use of electronic signatures, seems to be less than desirable. The substantially wider adoption of more interactive eHealth services among advanced users, compared to the other segments, may be largely attributed to the lack of clear standards and differences in the health-care systems of EU-15 countries, e.g., different regional, national, or European (health and eHealth) policies and regulations. Thus, a homogeneous European policy and legal framework is needed to further promote advanced eHealth applications, which provides clear guidelines on issues such as protection of electronic patient data, reimbursement schemes, or financial incentives for online patient communication. More sophisticated eHealth uses, such as telemedicine services, should be continually introduced to more advanced users at later stages.
With regard to the existence of national or regional differences in the use of Internet-based healthcare networks between European physicians, Northern European countries (Sweden, Finland, Denmark, and the United Kingdom) are clearly on the forefront, while Internet adoption by physicians from Southern countries (Greece, Spain, and Portugal) is clearly developing at slower paces.
As previously indicated, the observed differences in physicians' technology use across countries and type of eHealth application might be partly explained by the heterogeneity in the national health-care systems of EU-15 countries (European Commission 2008). Among others, health-care systems differ in terms of organization, e.g., the degree of centralisation of health systems, which may condition the number and variety of eHealth initiatives and interoperability of technological applications in each country; funding, such as the integration vs. exclusion of telemonitoring costs and online health advice from general reimbursement schemes; policy, i.e., national eHealth policies showing varying levels of maturity, scope, and sophistication; and legislation on relevant issues such as data protection, telemonitoring, eHealth service delivery, liabilities, or electronic health-care records.
Although more sophisticated eHealth uses, involving transfers of patient data online, can contribute to substantial improvements in the provision of patient care services (continuous patient monitoring, communication with patients, contact with dispensing pharmacists), the differences found between countries can limit the potential benefits of these Internet-related uses. Concerns about patients' privacy protection may slow down the adoption process of such Internet-based services in the health-care sector, and different national regulations in this matter are likely to widen regional disparities in the European Union. In this regard, the deployment of an interactive eHealth application, such as online prescriptions, is a reality mainly in (advanced) Northern European countries with a sophisticated eHealth strategy (e.g., Denmark and Sweden) (European Commission 2008). Conversely, (laggard) Southern countries like Greece and Portugal have recently developed or lack specific (policy and legal) frameworks for eHealth. Thus, generalisation of advanced eHealth services, such as online prescribing with full legal protection, is becoming a rather slow process.
It is also worth considering that the North/South divide in Internet adoption is also evident, not only among health professionals, but also with regard to the general public. If the potential of Internet technologies for improving the provision of patient care services is to be fully realised on a European basis, European and national authorities should play a key supporting role. The eEurope Action Plan 2005 and EU-Lisbon vision for 2010, with regard to the promotion of eHealth services, aim to build a homogeneous Europe-wide legal framework, which ensures the secure transfer of patient identifiable data over the Internet and dedicated healthcare networks (Cabrera et al. 2004). The commitment of national and regional authorities to these policies developed by the European Commission will be critical for their success.
Governmental support should mainly focus on promoting the adoption and use of Internet technologies (e.g., through marketing campaigns and training), developing modern digital infrastructures, and solving and clarifying the problems and risks associated by physicians and patients with the use of the Internet for health-related purposes (e.g., legitimate privacy and security concerns).
Previous research has suggested that the effects of external variables, such as demographics and geographic criteria, on Internet and eHealth usage may not be stable across different Internet and eHealth services (Burt and Sisk 2005; Korgaonkar and Wolin 1999). In general, these external variables have provided rather weak relationships with the identified segments in this research.
Of the analysed variables, only physicians' age showed a moderate association with the use of the Internet or a general practitioners network. Consistent with recent research (Audet et al. 2004; Brooks and Menachemi 2006; Garritty and El Emam 2006), a detailed analysis of relative distribution of eHealth user segments among different age groups revealed that age differences are most noticeable between physicians over 60 years and those in the lower age groups. The observed reduction in Internet and eHealth use among general practitioners over 60 years is likely to be the result of a cohort effect (rather than a real age effect) (Morris and Venkatesh 2000), resulting from older physicians' lower exposure to technology. According to these results, age differences in physicians' eHealth use may be regarded as a transitory situation.
Sex, location, and size of the medical practice have not provided significant effects on physicians' use of eHealth services. The non-existence of significant differences in the use of Internet-related technologies for health purposes, based on location of the medical practice has important implications, as eHealth services have a great potential for improving the protection of patients' health in rural and isolated areas. The prerequisite of the acceptance of Internet-based technologies by health-care providers in rural settings seems to have been achieved. In order to ensure the success of eHealth services in non-metropolitan areas, European, national, and regional authorities should further promote Internet use by citizens living in smaller towns and rural areas.
Future research could overcome some of the main limitations of this study and further clarify how the adoption of Internet-based networks is taking place in the health-care sector:
First, the use of perceptual and attitudinal measures towards the Internet and new digital technologies would offer a richer explanation of the relative role played by physicians' psychological characteristics in the adoption processes of Internet-based networks. Owing to the characteristics of the survey, the analyses were only based on behavioural and demographic measures.
Second, the use of secondary data involves several limitations, mainly related to the lack of flexibility in the measures to include in the study. Nevertheless, this lack of flexibility in study design is clearly balanced by the access to representative and comparative transnational survey data in all countries of the European Union (Eurobarometer database). Without access to this kind of large-scale secondary data source and due to the lack of the necessary financial and human resources, most researchers would not be able to carry out this kind of comparative research.
Thus, information researchers should place adequate value on publicly available datasets, such as those regularly provided by the Pew Research Center or the European Commission. Currently available Pew Internet and Eurobarometer datasets (Gesis 2009; Pew Research Center 2009) explore diverse topics pertaining to citizens' and professionals' adoption, use, attitudes towards, and purposes of information and communication technologies use (e.g., shopping, banking, health, or communication). In recent research (Martínez et al. 2007; Ortega et al. 2007), running similar analyses on Eurobarometer data to those performed in this study, i.e., cluster and regression statistical analyses, has proved useful in clarifying international research questions related to European citizens' usage of different digital services (e.g., developing suitable marketing strategies for online services such as Internet banking or online shopping).
Third, the increase in European physicians' eHealth use since 2002 is likely to have altered the structure and specific behavioural characteristics of the identified segments. According to a recent report (European Commission 2008), a positive evolution is especially observable in EU-15 general practitioners' online medical information searches, use of electronic health-care records, and, to a lesser extent, electronic transfers of patient identifiable data. Despite increasing usage rates for various eHealth services, a clear divide still exists between doctors mainly using the Internet for more basic purposes, such as seeking medical information, and those using the Internet or dedicated networks for more active and sophisticated purposes, such as providing electronic prescribing and telemedicine services, or exchanging e-mails with patients. Thus, the identified segment characterization continues to be useful for the development of eHealth promotion policies aimed at European physicians with differing eHealth-related attitudes and behaviour.
Finally, further research should analyse the acceptance of eHealth services by health professionals other than general practitioners, in order to obtain a better understanding of the adoption of Internet technologies in the health-care sector. A sample including surgeons, specialists, nurses, and other professionals would clarify if the acceptance of the Internet or dedicated healthcare networks is affected by the professional category of health staff.
The authors are very thankful to the Central Archive for Empirical Social Research (University of Cologne, Germany) for their support and providing access to the cross-national database used in this study. We are also grateful to the referees for their insightful suggestions and to Lauren Goodchild for her careful copy-editing work.
José Manuel Ortega Egea is an Associate Professor of Marketing in the Department of Business Administration, University of Almería, Spain. He received his PhD degree in 2008 from the University of Almería, Spain. His research areas include health information systems, technology acceptance, and e-marketing. José Manuel can be contacted at jmortega@ual.es
María Victoria Román González and Manuel Recio Menéndez are both Associate Professors of Marketing in the Department of Business Administration, University of Almería, Spain. They received their PhD degrees from the Complutense University of Madrid, Spain. María Victoria can be contacted a: mvroman@ual.es; Manuel can be contacted at: mrecio@ual.es
| Find other papers on this subject | ||
© the authors, 2011. Last updated: 17 February, 2011 |