Information Research
Special Issue: Proceedings of the 15th ISIC - The Information Behaviour Conference, Aalborg, Denmark, August 26-29, 2024
Digital health applications and health literacy: an explorative analysis
DOI: https://doi.org/10.47989/ir292833
Abstract
Introduction. In 2020, Digital Health Applications (known as DiGA) have been introduced to the German healthcare system. DiGA are medical devices based on digital technologies that can be prescribed by physician and psychotherapists and reimbursed by health insurance companies. DiGA must demonstrate a positive healthcare effect, e.g. by improving of health literacy. Health literacy as a concept has received increasing attention in recent years but has also been subject to a vivid debate on its theoretical underpinning and methodological challenges.
Method & Analysis. For this study, all 53 DiGA listed in the official registry were reviewed. We searched the DiGA registry to answer the following research question: do DiGA measure health literacy and which health literacy measurement instruments are applied?
Results. Of the 53 DiGA listed, 29 are permanently and 24 provisionally listed in the DiGA directory. Although seven DiGA use health literacy measurement tools, the theoretical or conceptual explanation of these tools and the decision to use them is lacking.
Conclusion. This paper argues that there is a need to empirically investigate the motivation of DiGA developers, taking into account the use and non-use of health literacy measurement tools.
Introduction
According to the World Health Organization (2024a) (WHO), ‘digital technologies are now integral to daily life, and the world’s population has never been more interconnected.’ Particularly in healthcare, digital health applications have the potential to empower consumers to manage and take responsibility for their health. In Germany, from 2020, it is possible that digital health applications (so-called DiGA, Digitale Gesundheitsanwendungen) can be prescribed by physicians or psychotherapists and will be reimbursed by health insurance companies. DiGA are lower-risk (class I and IIa) medical devices that are intended for patients as the primary user group and whose main function is based on digital technologies. All DiGA are listed and categorized in the DiGA directory, also providing additional information (e. g., price, ICD (The International Statistical Classification of Diseases and Related Health Problems) category) about the DiGA. In addition, the DiGA register (Bundesinstitut für Arzneimittel und Medizinprodukte, n.d.) is publicly available on the Internet so that anyone can access DiGA-related information. DiGA can be listed provisionally or permanently. To become listed a DiGA must undergo a certification process covering, among others, patient safety, functionality, and a positive healthcare effect (Bundesinstitut für Arzneimittel und Medizinprodukte, 28.12.2023). If a DiGA manufacturer was able to prove the general requirements but not the positive healthcare effect, a DiGA becomes listed provisionally and the manufacturer has one year to conduct a study showing the positive healthcare effect. One way of doing so is to improve the health literacy of the DiGA users.
(e-)health literacy has received much attention in the context of the increasing digitalization of healthcare. Sørensen et al. (2012, p. 3) explain that ‘[h]ealth literacy is linked to literacy and entails people’s knowledge, motivation and competences to access, understand, appraise, and apply health information in order to make judgments and make decisions in everyday life […]’. The concept has been criticized from several angles including a lack of theoretical underpinning and methodological issues (Max Planck Institute for Human Development, 2018; Sørensen et al., 2012; Wirtz and Soellner, 2022). Given that health literacy can play an important role in certifying DiGA, the question arises as to how developers make use of the concept. Some studies argue that DiGA offer the potential of increasing health literacy (Dahlhausen et al., 2021; Frey and Kerkemeyer, 2022). A study by Scheibe et al. (2023, p. 15) found that developers frequently use the concept, supposedly as it is ‘widespread and well-known outcome domain and various established outcome measurement instruments already exist in the form of validated questionnaires.’ However, to the best of our knowledge, no study has investigated which health literacy concepts were used by the DiGA developers.
We want to shed light on this question and want to give first insights to what extent the concepts have been integrated into DiGA. Hence our research question is:
RQ: Which health literacy measuring instruments were applied by DiGA manufacturers to prove the improvement of health literacy?
Health literacy
Over the past 20 years, health literacy become an increasingly important social and political issue (Okan and Pinheiro, 2020). There is no consistent conceptualisation or theoretical basis for the concept and when health literacy is viewed from an interdisciplinary perspective, the divergence is even greater. For example, in addition to health literacy, the term health information literacy is also used in the information science community. Hirvonen et al. (2016), Niemelä et al. (2012), and Shutsko (2022) conclude in their explanations that health information literacy can be seen as a conflation of health literacy and information literacy. A full discussion of the similarities and differences between health literacy and health information literacy is beyond the scope of this article. There are similarities between the concepts and Sørensen et al.’s (2012) definition is well-known. Since Hirvonen et al. (2020) refer to Huhta et al. (2018) who explain that Sørensen et al.’s (2012) view of health literacy ‘has brought also the operationalisation of the concept closer to that of health information literacy’, we decided to use this definition here.
In recent years, several instruments have been developed to measure health literacy (Kim and Xie, 2017). These instruments, however, are conceptually different and have emerged from multiple historical lines of development (Okan and Pinheiro, 2020). Examples of these instruments are the HLS-EU instrument, the Health Literacy Skills Instrument (HLSI), the Numeracy and Understanding in Medicine Questionnaire (NUMI), and the Health Literacy Questionnaire (HLQ) (Schwartz et al., 1997; McCormack et al., 2010; Osborne et al., 2013). Some of these instruments have been extensively debated. The HLS-EU was used to measure health literacy on a country level, carried out in several European countries. The main point of criticism here is the choice of questionnaire in the form of subjective assessment and the lack of psychometric verification (Max Planck Institute for Human Development, 2018; Wirtz and Soellner, 2022). Ngyuen et al. (2017) also emphasized that it is important to examine, among other aspects, the alignment of definition and measurement, validation methods, participant characteristics, and objective versus subjective measures of health literacy in order to obtain valid instruments that measure what they are supposed to measure. For example, a challenge with subjective instruments is that they do not measure the competence itself, but a self-assessment of one's own competence. This in turn can be influenced by socialization effects such as gender and social background (Ngyuen et al., 2017; Wirtz and Soellner, 2022).
Method
For this study all 53 DiGA listed in the official directory, as of January 15th, 2024, were reviewed by one of the authors (AI). We decided which search terms we were going to use, while checking the description and the studies if they were provided. We used the term health literacy (in English and German) to find first indications in the description that health literacy is considered as an endpoint to prove the positive healthcare effect by the DiGA developers. Figure 1 illustrates that the DiGA register offers several levels to obtain information about the DiGA (see Step 1, Step 2, Step 3). Those DiGA-related sub webpages within the here called DiGA Universe enable us to find at some steps new information. Before we started to review the DiGA we filtered the DiGA after provisionally and permanently listed. While checking those sub webpages (Step 1 - Step 3), we have collected information such as the name of the company, a description, the name of the DiGA, availability, whether the DiGA is provisionally or permanently listed and entered it into one excel file. Further, several DiGA register their pilot study or further studies within different registers for clinical trials. Therefore, if the registration IDs, for example, for the German Clinical Trials Register or for ClinicalTrials.gov were provided, those information were collected as well. Apart from the DiGA universe, we used those IDs to seek for further information considering the health literacy-related aspects if available (see Step 4). Additionally, there is also sometimes the opportunity to find publications at the DiGA webpages or via different sources, such as ResearchGate (see Step 5).
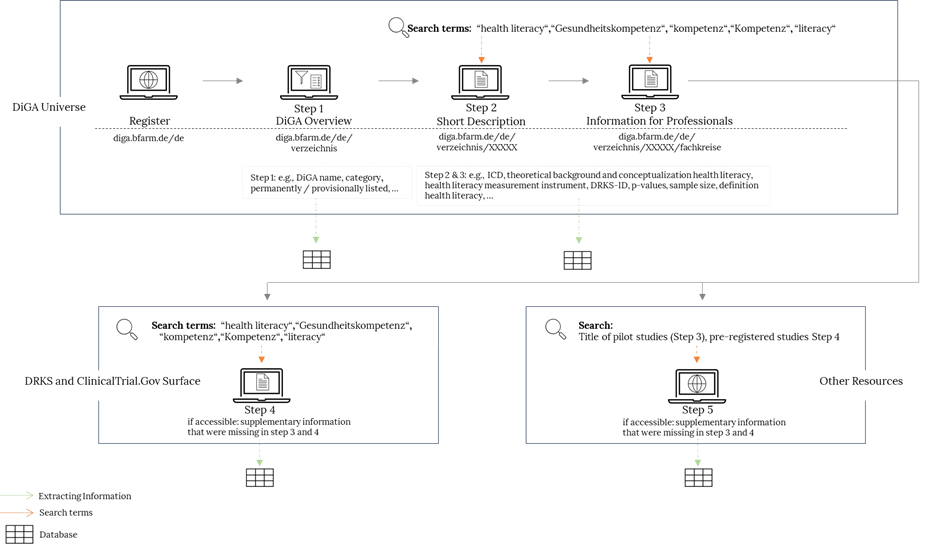
Figure 1. Search strategy and review process
Results
Of the total 53 listed DiGA, 29 have been permanently and 24 provisionally included in the DiGA directory. Seven of these 53 DIGA use health literacy as a secondary outcome and four of the seven DiGA are permanently listed. Of these seven, two were found to offer a service for patients with depression. Edupression.com provides information and psychoeducation for self-help, while elona therapy Depression offers psychological therapy that includes digital interventions and conversational therapy to support patients with unipolar depression. The other five DiGA that aim to improve health literacy have different areas of application, such as irritable bowel syndrome (Cara Care) or generalized anxiety disorders (Selfapys online course for generalized anxiety disorder). ProHerz (Heart) focuses on self-management and is characterized as an early warning system to detect changes in the disease by users themselves. NeuroNation MED aims to help patients alleviate symptoms of mild acquired or neurodegenerative cognitive impairment. PINK! is for women diagnosed with breast cancer. The PINK! DiGA accompanies users with questions about nutrition, exercise, and mental health. The instruments (see Table 1) employed to measure health literacy are just as diverse as the areas of application. Table 1 provides an insight into the extent to which health literacy (definition, concept and limitation) is mentioned by DiGA manufacturers within the DiGA register (DiGA universe). The DiGA that are permanently listed in the register illustrate the extent to which health literacy was increased (e.g., Cara Care, edupression.com) or not (e.g. Selfapys). PINK! has not yet provided any information regarding the proof of improvement of health literacy within the DiGA register.
| # | DiGA | Instrument | Definition | Concept | Limit. |
|---|---|---|---|---|---|
| 1 | edupression.com* | Depression literacy (D-Lit) | Yes | No | No |
| 2 | elona therapy Depression | Depression literacy (D-Lit) | No | No | No |
| 3 | Cara Care (for irritable bowel syndrome)* | HLS-EU16 | Yes | No | No |
| 4 | NeuroNation MED | Psychometric test (HLQ) | No | No | No |
| 5 | ProHerz (Heart) | Atlanta Heart Failure Knowledge Test (AHFKT) | No | No | No |
| 6 | Selfapys online course for generalized anxiety disorder* | Mental Health Literacy Scale (MHLS) | No | No | No |
| 7 | PINK!* | HLS-EU16 | No | No | No |
Table 1. Overview of the reviewed DiGA information; (DiGA marked with * are permanently listed in the DiGA directory)
Discussion and future research
The World Health Organization (2024b) emphasises that health literacy increases the empowerment of citizens. ‘[They] are enabled to play an active role in improving their own health, engage successfully with community action for health, and push governments to meet their responsibilities in addressing health and health equity’ (World Health Organization, 2024b). Although it is clear that health literacy has many benefits and healthcare professionals in Germany underline the advantages of improving health literacy (Dahlhausen et al., 2021; Frey and Kerkemeyer, 2022), this factor seems to be underutilized by DiGA developers if we consider the information provided within the DiGA directory. It must also be taken into consideration, that some data on health literacy has simply not yet been published. Overall, the analysis showed that at the time of the investigation only seven DiGA used health literacy as a secondary endpoint. Our initial findings confirm that various instruments are used to measure health literacy and that DiGA developer are also able to choose only certain items from the original measurement instruments. This can lead to bias in the results. It also leads to difficulties in the comparability of results, which is certainly relevant in a certification process. In order to be permanently listed in the DiGA directory, DiGA manufacturers must conduct clinical studies to prove the aforementioned healthcare effect. This requirement ensures that DiGA developers are able to measure the probable improvement in health literacy at the beginning and after a predefined period of time while using the defined measurement tool (e.g. questionnaire). During the review process we were also able to gain first insights that will be considered in future research, since these insights are in line with findings by Mäder et al. (2023), who explained that overall DiGA or rather the DiGA directory do not provide sufficient information regarding applied methodologies, a critical evaluation of the measures used, and reported results. In our systematic screening we were unable to find a comprehensive theoretical or conceptual discussion by DiGA developers with respect to the decision to apply measuring instruments for health literacy, with the exception of some information on the reliability of these instruments. However, as a standardized definition of health literacy does not yet exist, this is of great importance in the context of the current scientific debate (e.g., Nguyen et al., 2017). The jungle of health literacy concepts and measuring instruments, and the missing theoretical sharpness in the health literacy debate (Sørensen et al., 2012) may contribute to the current dearth of measuring health literacy as DiGA manufacturer.
Conclusion
The research process and results underline that the information provided by the DiGA registry lacks detail in this area and that there is a need to empirically investigate the motivations of DiGA developers regarding the use or non-use of instruments to measure health literacy. DiGA manufacturers are only one aspect of this critical discussion. Interviews with individuals responsible for the assessment of DiGA (e.g. Bundesinstitut für Arzneimittel und Medizinprodukte) could provide details on the relative attractiveness of tracking health literacy for DiGA developers, the challenges of concentrating on health literacy, and the depth of health literacy data that needs to be collected and reported. Furthermore, adding more extensive research information to the directory, such as the publications (published pilot studies within the journals or conferences) themselves and not only registered studies (e.g. the German Clinical Trials Register, the DRKS registry), could support not only researchers but also physicians and patients. On this basis, our future research should address DiGA developers’ background, professional knowledge and reasons for using health literacy instruments. These insights can contribute to the debate on health literacy in several ways: (1) by reducing the density of the conceptual and theoretical discussion of health literacy and (2) by clearly corresponding with the requirements for being permanently listed as a DiGA within the DiGA registry when health literacy is defined as an endpoint.
About the authors
Aylin Imeri (PhD) is a research associate at the Junior Professorship for Healthcare and E-Health at the Ruhr University in Bochum Germany. Her research is about self-tracking technologies in the health sector, health information, information behaviour, social media, human-computer interaction, motivation and gamification.
Sabrina Schorr (M.A.) is a research associate at the Junior Professorship for Healthcare and E-Health at the Ruhr University in Bochum. Her research is about quantitative social research, social inequality, digitalization, (digital) health literacy, sociology of technology, nursing, mental health and sociology of work.
Prof. Sebastian Merkel has been involved as a researcher in multiple national and international projects combining the fields of active and healthy ageing with both conventional and novel technological approaches. He is specialized in innovation research, particularly with respect to participatory approaches on technology development.
References
Bundesinstitut für Arzneimittel und Medizinprodukte (n.d.). Finden Sie die passende digitale Gesundheitsanwendung [Find the best fitting Digital Health Application]. Retrieved April 15, 2024 from https://diga.bfarm.de/de
Bundesinstitut für Arzneimittel und Medizinprodukte (28.12.2023). Das Fast-Track-Verfahren für digitale Gesundheitsanwendungen (DiGA) nach § 139e SGB V. Ein Leitfaden für Hersteller, Leistungserbringer und Anwender. (Version 3.5). [Report]
Dahlhausen, F., Zinner, M., Bieske, L., Ehlers, J. P., Boehme, P., & Fehring, L. (2021). Physicians’ attitudes toward prescribable mHealth apps and implications for adoption in Germany: Mixed methods study. JMIR mHealth and uHealth, 9(11), e33012. https://doi.org/10.2196/33012
Frey, S., & Kerkemeyer, L. (2022). Acceptance of digital health applications in non-pharmacological therapies in German statutory healthcare system: Results of an online survey. Digital Health, 8, https://doi.org/10.1177/20552076221131142
Hirvonen, N., Ek, S., Niemelä, R., Pyky, R., Ahola, R., Korpelainen, R., & Huotari, M. – L. (2016). Everyday health information literacy in relation to health behavior and physical fitness: A population-based study among young men. Library & Information Science Research, 38(4), 308-318. doi.org/10.1016/j.lisr.2016.11.013
Hirvonen, N., Enwald, H., Mayer, A.-K., Korpelainen, R., Pyky, R., Salonurmi, T., Savolainen, M.J., Nengomasha, C., Abankwah, R., Uutoni, W., Niemelä, R., & Huotari, M.-L. (2020), Screening everyday health information literacy among four populations. Health Information and Libraries Journal , 37, 192-203 e12304. doi.org/10.1111/hir.12304
Huhta, A. M., Hirvonen, N., & Huotari, M. L. (2018). Health literacy in web-based health information environments: Systematic review of concepts, definitions, and opera-tionalization for measurement. Journal of Medical Internet Research, 20(12), e10273. doi.org/10.2196/10273
Kim, H., & Xie, B. (2017). Health literacy in the eHealth era: A systematic review of the literature. Patient Education and Counseling, 100(6), 1073–1082. https://doi.org/10.1016/j.pec.2017.01.015
Max Planck Institute for Human Development (2018). Unstatistik des Monats: 54 Prozent der Deutschen haben eingeschränkte Gesundheitskompetenz. Die Unstatistik des Monats Februar beschäftigt sich mit der vermeintlichen Gesundheitskompetenz der deutschen Bevölkerung. https://www.mpib-berlin.mpg.de/unstatistik-vermeintliche-gesundheitskompetenz
Mäder, M., Timpel, P., Schönfelder, T., Militzer-Horstmann, C., Scheibe, S., Heinrich, R., & Häckl, D. (2023). Evidence requirements of permanently listed digital health applications (DiGA) and their implementation in the German DiGA directory: an analysis. BMC Health Services Research, 23(1), 369. https://doi.org/10.1186/s12913-023-09287-w
McCormack, L., Bann, C., Squiers, L., Berkman, N. D., Squire, C., Schillinger, D., Ohene-Frempong, J., & Hibbard, J. (2010). Measuring health literacy: a pilot study of a new skills-based instrument. Journal of Health Communication, 15(2), 51–71. https://doi.org/10.1080/10810730.2010.499987
Nguyen, T. H., Paasche-Orlow, M. K., McCormack, L. A. (2017). The State of Science of Health Literacy Measurement. Studies in Health Technology and Informatics, 240, 17-33.
Niemelä, R., Ek, S., Eriksson-Backa, K., & Huotari, M. -L. (2012). A screening tool for assessing everyday health information literacy. Libri, 62(2), 125–134. doi.org/ 10.1515/libri-2012-0009
Okan, O., & Pinheiro, P. (2020). Von Chicago 1958 bis Shanghai 2016: Ein Rückblick auf zentrale Entwicklungstrends in der Geschichte der Gesundheitskompetenz. In T. M. Bollweg, J. Bröder, & P. Pinheiro (Eds.), Health Literacy im Kindes- und Jugendalter (pp. 11–38). Springer Fachmedien.
Osborne, R. H., Batterham, R. W., Elsworth, G. R., Hawkins, M., & Buchbinder, R. (2013). The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health, 13, 658. https://doi.org/10.1186/1471-2458-13-658
Scheibe, M., Knapp, A., Harst, L., & Schmitt, J. (2023). Outcome domains and measurement instruments of patient-relevant improvement of structure and processes as a new set of outcomes for evaluating and approving digital health applications: systematic review. Discover Health Systems, 2(33). doi.org/10.1007/s44250-023-00046-6
Schwartz, L. M., Woloshin, S., Black, W. C., & Welch, H. G. (1997). The role of numeracy in understanding the benefit of screening mammography. Annals of Internal Medicine, 127(11), 966–972.
Shutsko, A. (2022). Country-specific digital inequalities in older people’s online health information seeking in europe: Impact of socio-demographic and socio-economic factors. Journal of Information Science Theory and Practice, 10(4), 38-52. doi.org/10.1633/JISTaP.2022.10.4.4
Sørensen, K., van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., & Brand, H. (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12(80). https://doi.org/10.1186/1471-2458-12-80
Wirtz, M.A. & R. Soellner, 2022: Gesundheitskompetenz. Diagnostica 68, 163–171. https://doi.org/10.1026/0012-1924/a000299
World Health Organization (2024a). Digital Health. https://www.who.int/health-topics/digital-health
World Health Organization (2024b). Health Promotion. https://www.who.int/teams/health-promotion/enhanced-wellbeing/ninth-global-conference/health-literacy