Information Research
Special Issue: Proceedings of the 15th ISIC - The Information Behaviour Conference, Aalborg, Denmark, August 26-29, 2024
Development in the adoption of a national digital healthcare system and experience at taking new technology in use – changes from 2019 to 2022
DOI: https://doi.org/10.47989/ir292841
Abstract
Introduction. The adoption of a national digital system for healthcare services in Iceland, and how people perceive their possibilities to adopt new technology is examined.
Method. Surveys using random samples of people aged 18 years and older were conducted. The samples consisted of 1.800 people in 2019 and 1.200 in 2022. People 18-59 years old were reached by emails and 60 or older by phone. Response rates were 39% in 2019 and 45% in 2022.
Analysis. The analysis is descriptive. Survey results from 2019 and 2022 are compared and differences by sex and age examined.
Results. Considerable change was detected in use of the system for communication with health professionals tailored to participants health, while no increase was in obtaining information regarding issues not directly connected to people’s health history. The possibilities of adopting health technology were considered substantially better in 2022 than in 2019.
Conclusion. People are likely to use digital healthcare systems when the situation requires, and they receive necessary support. It is important to consider the needs of those who are getting older for people to have equal opportunity to benefit from digital health information. Furthermore, reliable information offered by health professionals need to be promoted.
Introduction
It is essential that people have access to quality information in relation to their own health and other health related issues so that they can make knowledgeable health decisions. Information and communication technology can open possibilities for people to retrieve information that are relevant to their needs, as well as offering new ways to communicate with health professionals.
In recent years, the attention has increasingly focused on the use of information and communication technology within healthcare services, and the possibilities that it can bring. A better understanding of the growth in the use of it and the factors that can influence the adoption of it, has been called for (da Fonseca et al., 2021).
The World Health Organization (2021) has put forward a global strategy of digital health 2020-2025, with the aim of strengthening health systems by the use of information and communication technologies for the public. The purpose is to empower individuals and promote their health and wellbeing through the use of technological solutions. The strategy, furthermore, acknowledges that to achieve the vision of health for all, the focus needs to be on people and their adoption of health information and communication technology.
The question, however, remains whether everyone has an equal opportunity to benefit from health digitalisation and take advantage of it to improve their health.
The current paper examines health information behaviour of people at the age of 18 years and older in relation to progress in the adoption of a national information and communication system used for digital healthcare services in Iceland, as well as how people perceive their possibilities to adopt new technology. Results from surveys conducted in 2019 and 2022 will be compared, thus the focus will be on the development that has happened in this period. Furthermore, differences by sex and age will be examined.
Reference review
The options of producing, disseminating, and accessing health information have been rapidly changed by information and communication technology, a development that can be expected to continue in the coming years. People are constantly required to adjust to and learn about recent advances in their information environment.
The use of information and communication technologies for healthcare services has attracted a growing interest in the past years. It has been pointed out that it is possible to use it to bring the healthcare system closer to people. For example, poor accessibility because of geographical isolation, or other difficulties that make it problematic for people, or even hinders them, in using healthcare service on-site, can be countered by the use of information and communication technology (Alvarez, 2002; Shao et al., 2022).
Previous studies have reported about favourable use of health technology for communication and support by healthcare professionals (Tapuria et al., 2021). It has been mentioned that individuals can be empowered to become more involved in their own healthcare through enhanced digital information and communication exchange between them and healthcare professionals, with information that is tailored to the needs of the individual (Lindberg et al., 2013; World Health Organization, 2021). Thus, a relationship which is based more on partnership and mutual decision making may become possible, which in turn can improve the quality of the healthcare service (Eysenbach, 2001).
The importance of promoting digital healthcare services was evident well before COVID-19 broke out, however, the significance of it for health information exchange between individuals and healthcare professionals became even more apparent at the outbreak of the pandemic in 2020 (Budd et al., 2020). In response to the pandemic, and in order to limit the possible transmission of infection and the risk of COVID-19, people in various countries were recommended to use information and communication technology for communication, rather than visiting healthcare clinics (Ortega et al., 2020; Bhaskar et al., 2020; Murphy et al., 2021).
Researchers that investigate the acceptance of health information technologies have used various theories (Chong et al., 2022), however, the technology acceptance model (TAM), as well as the unified theory of acceptance and use of technology (UTAUT), and the theory of planned behaviour (Chong et al., 2022; Tao et al. 2020), have been identified as the most dominant theories, with TAM being the one most widely applied (Tao et al. 2020). TAM consists of five core constructs, that is: perceived ease of use, perceived usefulness, attitude, behavioural intention and actual usage behaviour. Of those, attitude was not included in a later update of the theory, TAM2, while subjective norm (social influence) was added to it (Tao et al. 2020). The unified theory of acceptance and use of technology (UTAUT) builds on some of the same core constructs as TAM2, although they are classified under different phrases. UTAUT suggests that the actual use of technology is determined by behavioural intention, which in turn is directly affected by four constructs: performance expectancy (usefulness by TAM, TAM2), effort expectancy (ease of use by TAM, TAM2), social influence, as well as facilitating conditions which refers to peoples experience of resources that they can draw upon to get support at using technology. In addition, the model proposed the moderators age, gender, experience and voluntariness of use, that can define the strength of predictors on intention (Venkatesh et al., 2003).
Although studies have found that healthcare information and communication technology can benefit people in various ways it is known that it can also pose challenges (Arsad et al., 2023). Gu et al. (2021) have found several factors that can have positive effects on people’s willingness to engage in using digital healthcare systems. That includes the belief that it will satisfy their need for information, and that the use of it will be beneficial and valuable for them. Thus, the information that is available and how they are being promoted is of significance. Likewise, Crameri et al., (2022) found that how people perceive the benefits of adopting health technology to be of importance.
Socio-demographic characteristics have also been pointed out as an important factor when it comes to the use or non-use of digital health information (Ali et al., 2020). Crameri et al., (2022) identified several factors, for example age, income, employment status, educational level and health status.
Age has repeatedly been related to health information with studies indicating that older people have fewer digital skills than those who are younger. Older people have for example been found to use health information, as well as healthcare services, more than those who are younger (Jørgensen et al., 2016; Singh et al., 2018). However, when it comes to interest in using digital health information, those who are at the age 45-65 years have been found to show more interest in it than those who are older (Gordon and Crouch, 2019). Furthermore, those who are 40 years of age and older have been found to be less likely to use digital health information than those who are younger (Ali et al., 2020). In addition, age has been reported to be associated with the use of digital healthcare services, with those who are younger using it more frequently than those who are older (Sun et al., 2019; Sana et al., 2022). It has also been noted that social and cultural aspects of age matter (Helsper and Reisdorf, 2017). For older adults, it is important that they possess the informational and technological competence which is needed to take advantage of health information and communication technology (Bol et al. 2016). Furthermore, being able to get information as needed about how to use technology is important (Holko et al., 2022). It is essential that people are confident that they have the support which is necessary for taking technology into use (Anderson and Perrin, 2017). This is particularly vital for older adults who may need to rely on assistance from relatives, even though they find it difficult to ask them for help and may have a certain reluctance to do so (Pálsdóttir, 2012a; Pálsdóttir, 2012b).
Helsper and Reisdorf (2017) pointed out that education is an increasingly important variable, with those who have a higher level of education being much more likely to use digital sources in general than those who have a lower level of education. This is in line with results reported by other studies that have found people with higher education using more digital health information sources than people with lower education (Ali et al., 2020). Likewise, it has been found that people with lower education are less likely to use digital devices to be in contact with health professionals, as well as using digital health information, than those with higher education (Kontos et al., 2012).
Furthermore, previous studies have reported that sex is associated to the use of healthcare services, with women utilising it more than men (Jatrana and Crampton, 2009; Jørgensen et al., 2016; Singh et al., 2018), including the use of digital healthcare service (Sana et al., 2022). In addition, women have been found to seek digital health information more frequently than men (Bidmon and Terlutter, 2015; Escoffery, 2018; Hallyburton and Evarts, 2014), as well as using healthcare technology such as apps more than men do (Escoffery, 2018; Sana et al., 2022), and use technology to be in contact with health professional more than men (Kontos et al., 2014).
For people to be able to actively manage their health and improve their health behaviour and wellbeing, it is imperative that they can access quality health information that satisfy their needs. It has been reported to hold several benefits for people, such as leading to better health knowledge, improvements in health behaviour, and engagement in self-management (Tapuria et al., 2021). A better understanding of the growth in the use of healthcare information and communication technology and the factors that can affect the adoption of it has been called for (da Fonseca et al., 2021)
Because of a widespread access to the Internet in Iceland (Statistics Iceland, 2014) the conditions for obtaining digital health information can be considered excellent. It, nevertheless, needs to be kept in mind that access to the Internet does not necessarily translate into the use of digital health information (Ono and Zavodny, 2007). Therefore, other aspects related to the use of health technology need also to be considered. Steps have been taken to improve people’s access to health information in Iceland. In 2009, a new legal framework was set to ensure people the right to access to their health history through their health records. Many of the files are, however, not yet in a digital form (Health Records Act, 2009). Furthermore, a digital information and communication system, which is a multipurpose tool, has been developed. The system's website offers access to a wide range of various information from health professionals, about diseases, health issues and healthy lifestyle. Thus, users are allowed the opportunity to seek, examine, and gain knowledge from reliable health sources, through the website. The system is also a communication system for health professionals and the users. This part of the system offers various functions that provide a possibility for people to get various health information that are tailored to their own needs. It allows people, for example, to book appointments with their physicians or other health specialists, drug prescriptions can be examined and requests for renewal sent, history of vaccinations can be observed, and short questions or comments can be sent to physicians and answers from them received. In addition, a health professional is available for webchat during opening hours. Some parts of people’s health history are already being recorded into the system daily, while other types of access are still under development. This includes for example health records made during doctors’ appointments, which are not accessible yet through the system (Directory of health, 2016).
Aim and Research Questions
Based on the discussion above, the study aims to explore the adoption of a national digital healthcare system, as well as the experience of the possibilities to adopt information and communication technology, among Icelanders´ aged 18 years and older. Data that was gathered in 2019 and in 2022 will be compared to reveal possible changes during this period. The following research questions were asked:
How has the adoption of the national digital healthcare system developed in the period 2019 to 2022, and how does it relate to age and sex?
How has peoples experience of adopting new information and communication technology and receiving help at using it developed in the period 2019 to 2022, and how does it relate to age and sex?
The purpose of addressing this is to understand better how people can benefit from development in health information and communication technology to seek information about their own health, and thereby enhance their abilities to adopting healthier lifestyle. A better understanding of factors that relate to this can have implications for digital healthcare services and be used by health professionals and health authorities to work on improvements as needed.
Methods
Quantitative methods were used, and surveys conducted in 2019 and 2022.
Data collection
For each survey, the data were gathered from two random samples from the National Register of Persons in Iceland, using internet and telephone surveys. The surveys were conducted in January 2019 and in July 2022. In 2019 the total sample size was 1.800 people, 18 years and older. For the telephone survey, a random sample of 300 people aged 60 years and older was used, while for the internet survey a random sample of 1.500 people at the age of 18 to 59 years was used. In 2022 the total sample consisted of 1.200 hundred people, 18 years and older. The telephone survey used a random sample of 300 people aged 60 years and older and for the internet survey a random sample of 900 people at the age of 18 to 59 years was used. For the telephone surveys in both years, samples randomly selected from the National Register of Persons in Iceland were used. For the internet surveys, random samples from the Social Science Research Institute at the University of Iceland net panel, was used and people contacted by email. The net panel is based on a random sample from the National Register of Persons in Iceland and consists of people aged 18 years or older from the whole country who had agreed to participate in online surveys organised by the organisation. The choice of participants in the net panel follows strict methodological rules to avoid convenience sampling. The net panel is updated regularly to ensure that it corresponds with the distribution in the population, regarding sex, age, and residence.
For the surveys each year, both datasets (internet and telephone surveys) were merged, allowing answers from all individuals belonging to each set of data. The total response rate was 39% in 2019 and in 2022 it was 45 %.
Measurements and data analysis
In addition to the background variables, sex, age, education and residence, the measurements for the part of the surveys presented in the paper consisted of four questions that were examined in 2019 and in 2022:
The use of the digital healthcare information and communication system was examined by two questions. A five-point response scale was used for both questions (Very often – Never):
The participants use of the national healthcare system in relation to their own health was examined by the question: How often or seldom have you used Heilsuvera to communicate with health professionals or to get information about your own health (e.g. due to appointments, renew drug prescriptions, or send a message to your family physician).
The use of the system to seek information about various health issues was examined by the question: How often or rarely have you used Heilsuvera to get information about a healthy lifestyle, such as nutrition or exercise, or other health related issues?
The possibilities of taking new health information and communication technology in use were examined by two questions which were in the form of statements. A five-point response scale was used for both statements (Strongly agree – Strongly disagree):
I find it difficult to adopt new technologies.
I can easily get help using information and communication technology if needed.
Because of the response rate in the studies, the data for both years were weighted by sex (male, female), age in six categories, residence (within or outside the capital area) and education (primary, secondary, university) of participants so that it corresponds with the distribution in the population. Reference figures for age, sex and place of residence were obtained from the National Registry of Iceland and for level of education from Statistics Iceland. Raking method was used, with 5 as upper limit and 0.2 as lower limit. The analysis of the data is descriptive, and all analyses are based on weighed data. Based on previous analyses of the data it was decided to use sex and age for the examination. Survey results from 2019 and 2022 will be compared.
Results
Two questions examined participants use of the national healthcare system. One of the questions asked how often they had used it for activities such as to communicate with health professionals to get information in relation to their own health (e.g. booking appointments, renewing prescriptions, or sending messages to their physician). In addition, they were asked about their use of the system to seek information about various health issues, such as nutrition and exercise, or other health related issues. The results are introduced in Figures 1 and 2.
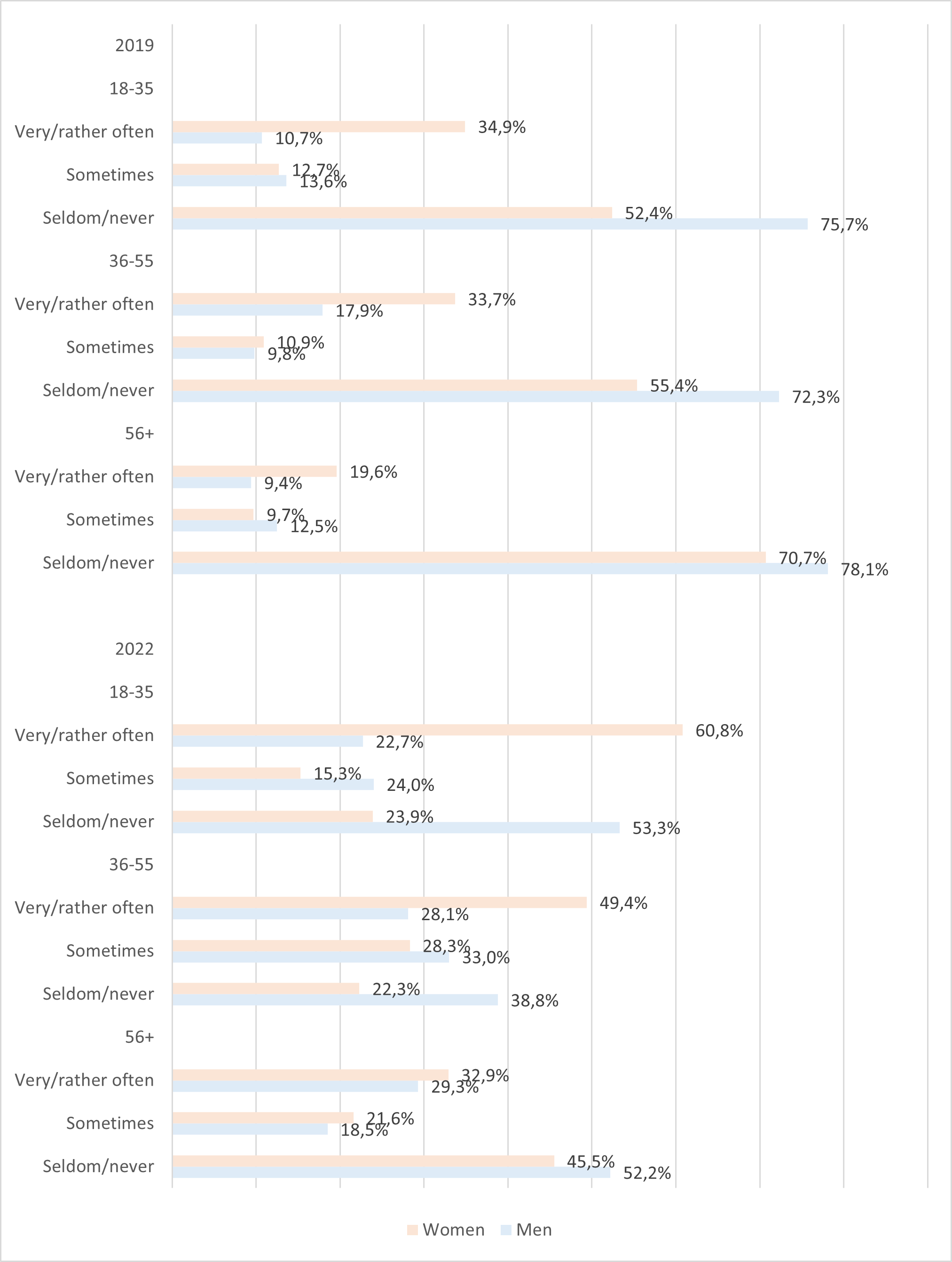
Figure 1. How often or seldom have you used Heilsuvera to communicate with health professionals or to get information about your own health (e.g. due to appointments, renew drug prescriptions, or send a message to your family physician)
Figure 1 shows that in 2019, participants in all age groups had not used the system much to communicate with health professionals or for other purposes related to their own health. Women in the oldest group were less likely to have used it than those in the two younger groups, where the usage across age groups was similar. The use by men, on the other hand, was quite similar across all three age groups. There was a difference by sex. Women in the age groups 18-35 (p <0.001) and 36-55 (p <0.10), had used the system significantly more often than men. In addition, women in the oldest group had used it more than men but the difference between them did not reach significance (p = .108).
In 2022, on the other hand, there was a considerable change in use of the system. Although majority of men in both the youngest and the oldest age group still used it seldom or never, the results nevertheless reveal that there is a substantial increase in the use of it for both men and women in all age groups. There was a significant difference by sex in the age groups 18-35 (p <0.001) and 36-55 (p <0.10), with women using it more than men. Even though women in the oldest group had used it somewhat more often than men, the difference was not significant (p = .663). Furthermore, there was an age difference for women, the majority of women in the youngest group and close to half of those aged 36 to 55 years had used it very or rather often, and this was also found for more than third of women in the oldest group. For men, however, there is much less difference by age, and in particular the use of the system by men in the youngest and the oldest age groups is quite similar (Figure 1).
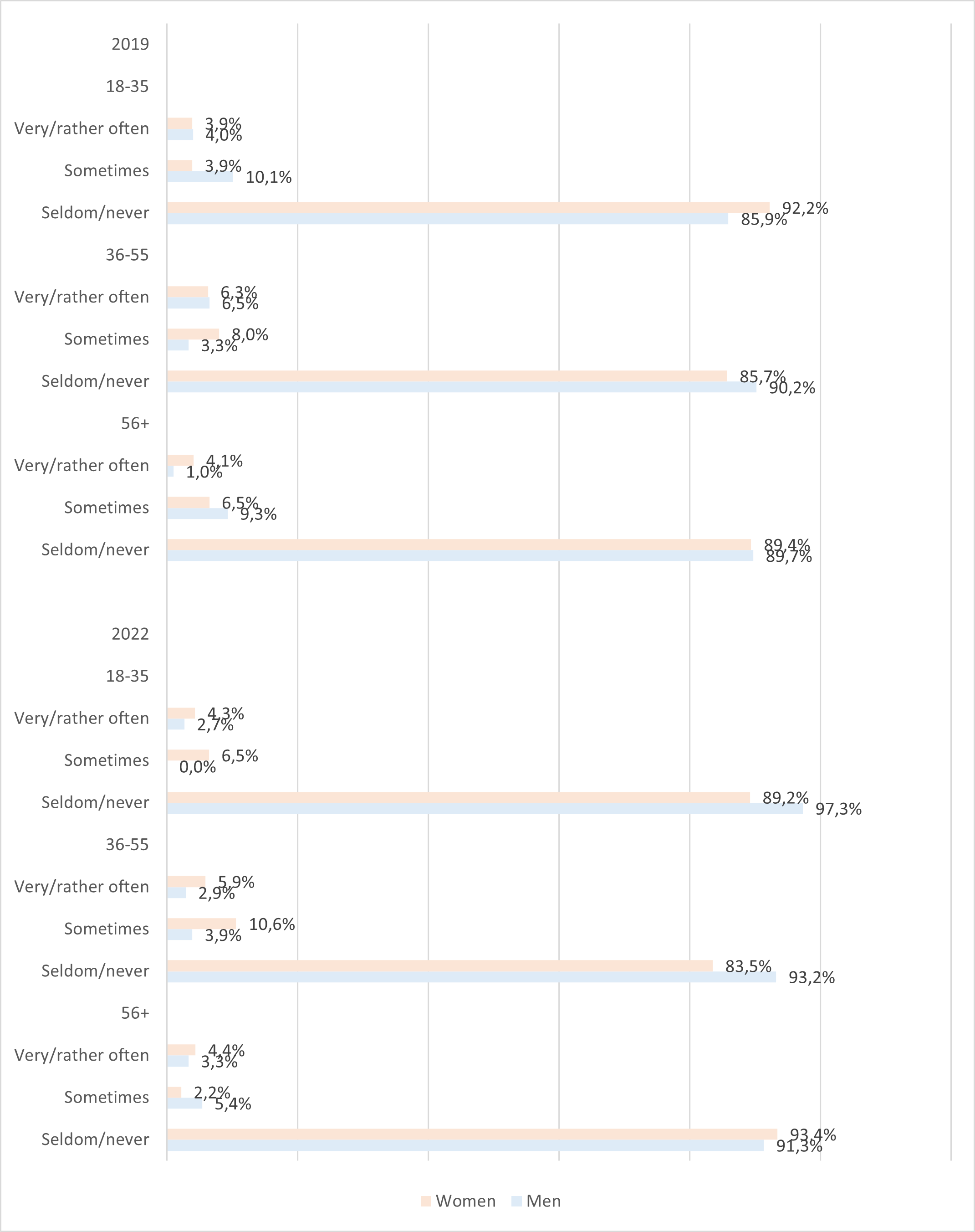
Figure 2. The use of the system to seek information about various health issues was examined by the question: How often or rarely have you used Heilsuvera to get information about a healthy lifestyle, such as nutrition or exercise, or other health related issues?
As can be seen in Figure 2, participants of both sexes, in all age groups, rarely sought information about healthy living and other health issues through the system in 2019. No significant difference was found by sex (18-35, p = .191; 36-55, p = .277; 56 and older, p = .306). Furthermore, the use of the system continued to be very low in 2022 and was almost identical to what it was as in 2019. No significant difference was found between men and women (18-35, p = .066; 36-55, p = .106; 56 and older, p = .495).
In addition, the participants were asked about how difficult it had been for them to adopt new information and communication technology, and about their possibilities of getting assistance at using technology. Results about the statement “I find it difficult to adopt new technologies” are presented in Figure 3.
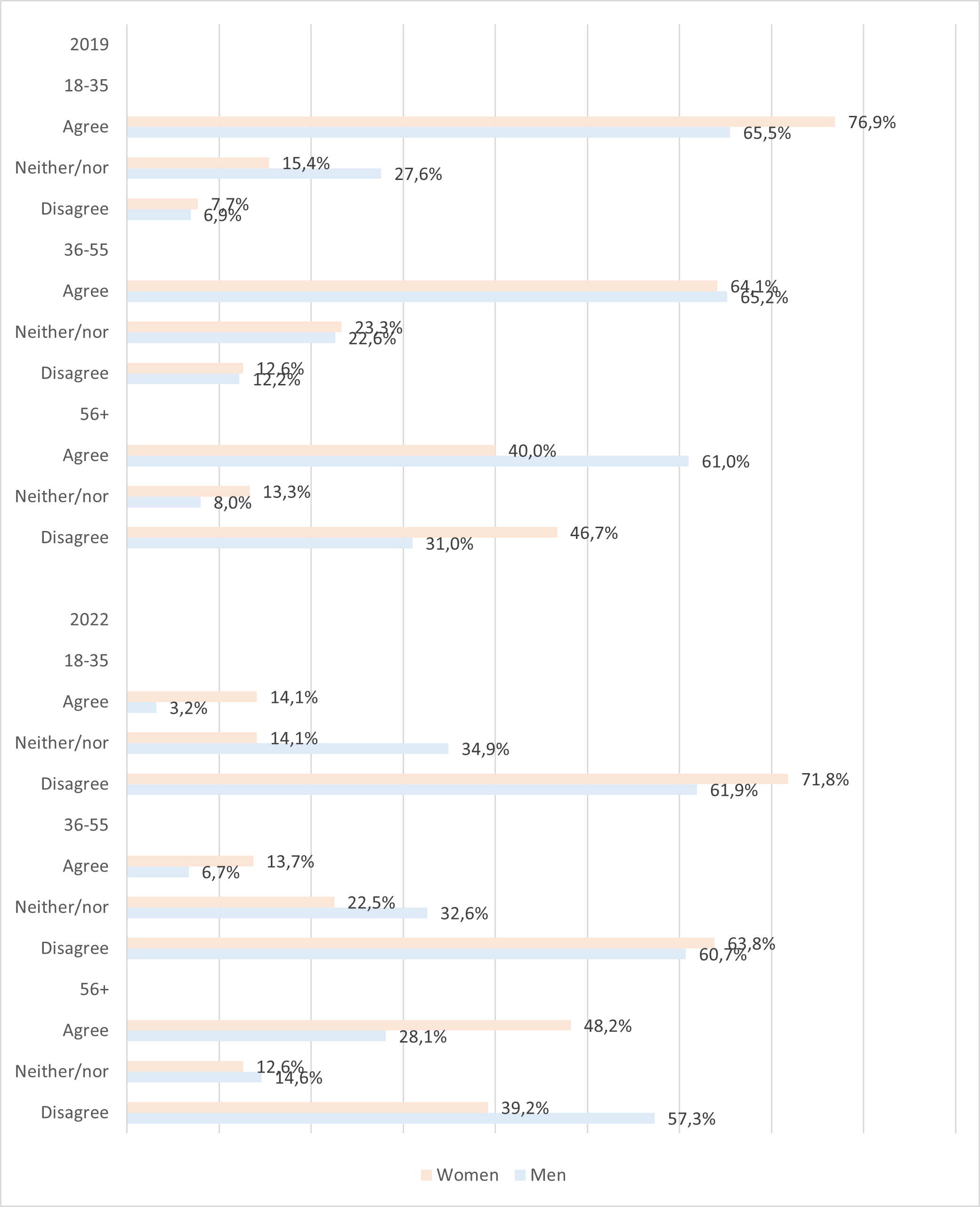
Figure 3. I find it difficult to adopt new technologies
Figure 3 shows that there are considerable changes in how people perceived their possibilities of adopting health information and communication technology, with a lower percentage of participants experiencing difficulties at it in 2022 than in 2019. In 2019, no difference was found by sex in the two younger groups (a 18-35, p = .111; 36-55, p = .985), with majority of both men and women finding it difficult to start to use new health technology The same was found for men in the oldest group, while women found it significantly less difficult (p < .010). In 2022, however, the results were reversed for all groups, except for women in the oldest age group. Majority of both men and women in the two younger groups disagreed that adopting new technology was difficult. There was a significant difference in the age group 18-35 (p < 0.001), with women being more likely to be in a disagreement than men, as well as in the group 56 years and older (p < 0.010), where men were more likely to be in a disagreement. No significant difference was detected for the age group 36-55 (p = .160).
In addition, results about the statement “I can easily get help at using information and communication technology if needed” are introduced in Figure 4.
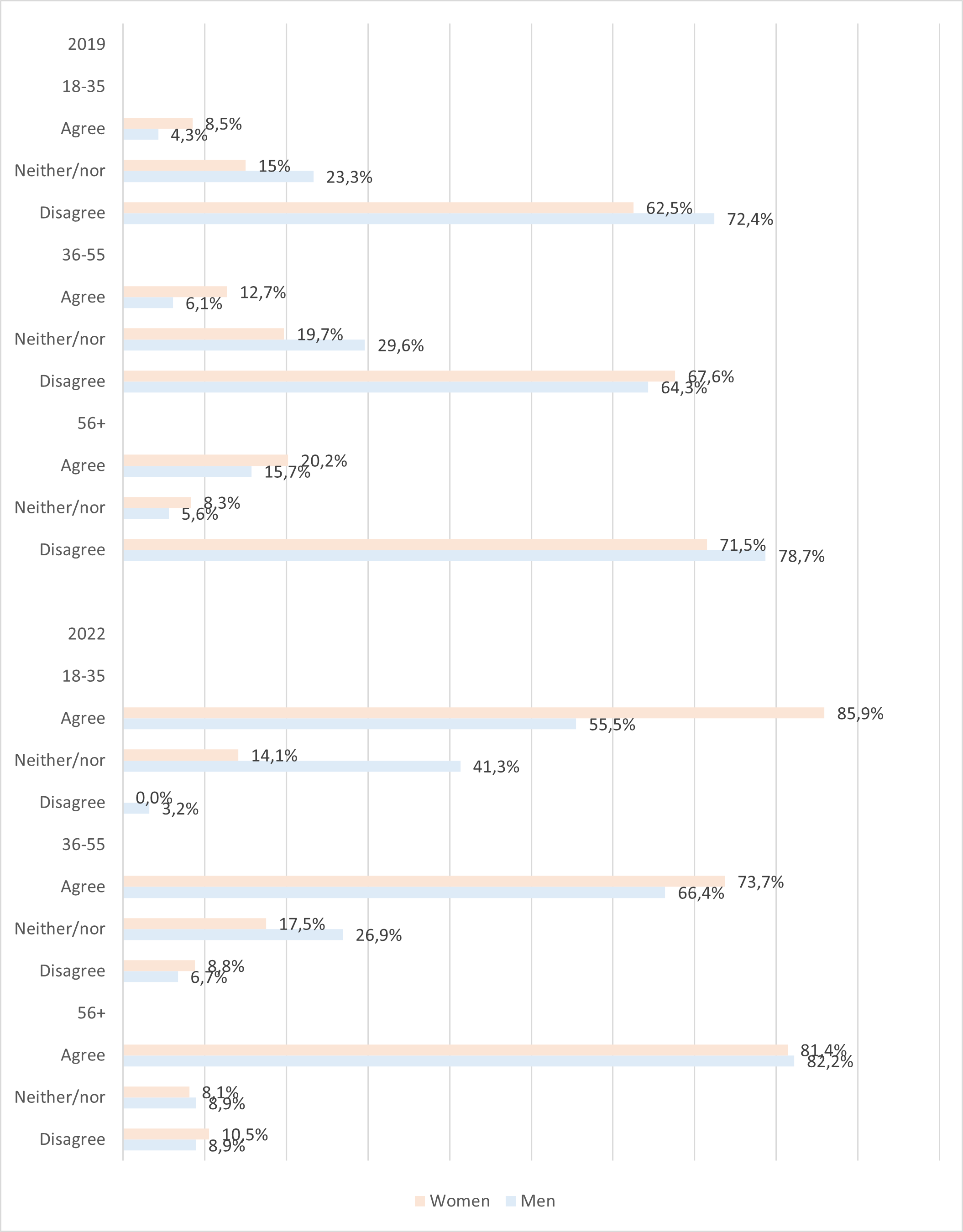
Figure 4. I can easily get help at using information and communication technology if needed
The results in Figure 4 show that there was a huge change in how participants in all groups assessed their potential of getting assistance at using information and communication technology. In 2019 the majority of participants in all groups disagreed with the statement “It is easy for me to get help at using information and communication technology if needed”. Although men in the youngest (p = .228) and the oldest groups (p = .510) are somewhat more in disagreement than women the results were not significant. Likewise, results for the group 36-55 years old (p = .089), when women were slightly more in disagreement were not significant.
The results were, however, reverse in 2022, with majority of participants in all groups agreeing that it is easy for them to get help. There was a considerable and significant difference by sex in the youngest group (< 0.001), with women finding it easier to get help than men. In addition, women in the group 36-55 years old were somewhat more in agreement than men but the difference was not significant (p = .327), while for the oldest group there was not a difference by sex (p = .930). (See Figure 4).
Discussion
Progress in digital health for the public and the opportunities of all groups within society to benefit from it has attracted increasing attention in recent years. By comparing results from surveys conducted in 2019 and 2022 the study examined the development in the adoption of a national system used for digital healthcare services by different groups in Iceland, as well as how people perceived their possibilities to adopt technology.
Two research questions were developed for the study. The first one asked: How has the adoption of the national digital healthcare system developed in the period 2019 to 2022, and how does it relate to age and sex?
A considerable change was detected in the use of the system for communication with health professionals or other purposes related to their own health. In 2019, both men and women in all age groups had not used the system much for this, while in 2022 there was a substantial increase in the use of it by all groups. There was a difference by sex, with women using the system more than men. The difference was significant for the age groups 18-35 and 36-55 years but did not reach significance for those aged 56 years and older. This is in line with what previous studies have reported about women using digital healthcare technology and service more than men (Escoffery, 2018; Kontos et al., 2014; Sana et al., 2022), as well as seeking digital health information more frequently (Bidmon and Terlutter, 2015; Escoffery, 2018; Hallyburton and Evarts, 2014). In addition, prior studies have identified age as a factor (Crameri et. al, 2022). Studies indicate that despite older people are more in need for health information and healthcare services than those who are younger (Jørgensen et al., 2016; Singh et al., 2018), they are less likely to make use of digital healthcare services (Sun et al., 2019; Sana et al., 2022). The current study supports this for women, as in both 2019 and 2022, those in the oldest age group had used the healthcare system less often than younger women. The results, however, do not show and age differences by men.
The low use of the healthcare system for information tailored to people’s health and communication with health professionals in 2019 may be explained by it not having been introduced much. In most of the health clinics in Iceland the system had been in use for a relatively short time. Considering that when a new system is put into use it takes some time, first of all, to introduce it to people, and secondly to engage people in adopting it, it is not particularly surprising that it was used so rarely. When Covid-19 happened in 2020 more was done to promote the system and the pressure on people to use it increased. This is similar to what was done in various other countries, where people were encouraged to use information and communication technology for health communication, rather than visit healthcare clinics on-site (Ortega et al., 2020; Bhaskar et al., 2020; Murphy et al., 2021). The system was used to promote information about Covid-19, for example to book appointments for testing for Covid-19, for receiving test results, and to order certificates. And on the whole people were recommended to use it more, not only for information about Covid-19 but for information related to their health in general. Thus, the explanation for the increased use of the system can, at least partly, be the fact that people were advised, if possible, to use it rather than visiting the health clinics.
Results about development in the use of the system for obtaining various high quality information regarding issues that are not directly connected to people’s health history, however, show that there was no increase in the use of it. For all groups, the results show that both in 2019 and 2022, information about healthy living and other health issues were rarely sought. Health institutions have emphasised the importance of people using reliable information (Dramé, 2020; World Health Organization, 2020). Because the system offers trustworthy information from health professionals that can be used to make informed decisions about healthy living it is essential that health authorities put an effort into introducing this part of the system better.
The perceived ease of using technology, or expected effort at adopting it, is among the core constructs in the technology acceptance model (TAM, TAM2) and the unified theory of acceptance and use of technology (UTAUT) (Tao et al., 2020; Venkatesh et al., 2003). Furthermore, to encourage adoption of health information and communication technology people need to be helped to deal with various challenges that come with new technology. Among other things, it has been noted that they must be convinced that the use of it will provide them with valuable information tailored to their own needs, and that it will be beneficial for them to adopt it (Arsad et al, 2023; Gu et al., 2021). The significance of this is, furthermore, emphasised by the inclusion of it as core constructs in both TAM, TAM2 (Tao et al. 2020) and UTAUT (Venkatesh et al., 2003). In addition, the UTAUT model defined facilitating conditions as a core construct. This refers to people’s perceptions of the support that is available for them at using technology (Venkatesh et al., 2003). Moreover, the importance of people having access to help at taking technology in use, particularly those who are older, has been stressed by other studies (Anderson and Perrin, 2017; Pálsdóttir, 2012a, 2012b).
The second research questions of the study asked how peoples experience of adopting new information and communication technology and receiving help at using it had developed in the period 2019 to 2022, and how it relates to age and sex. The results show that there was a huge change in how people perceived their chances of adopting new technologies.
Participants in all groups, except women in the oldest age group, were considerably less likely to find it difficult to take new information and communication technology in use in 2022 than in 2019. An age difference was found by women. In 2019 those in the youngest group were most likely to find this difficult and those in the oldest group least likely. In 2022, however, the results were reverse, with women in the youngest group were least likely to consider it difficult, and those in the youngest group most likely to do so. No age difference was, on the other hand, detected for men, with the results for them being identical, both in 2019 and in 2022. In addition, although there was some significant difference by sex the results were rather mixed and difficult to interpret.
Furthermore, participants in all groups deemed their chances of getting help at using technologies to be considerably better in 2022 than in 2019. Some differences were detected by age. In 2019, people in the oldest group were more likely to consider it difficult to get assistance than the younger groups. In 2022 there was an age difference by men, as the older they were the easier they considered it to get help. Age difference by women was not as pronounced, although women at the age 36-55 years were somewhat less likely to find this easy than those in the other two age groups. In addition, in 2022 there was a considerable difference by age in the youngest group (18-35 years, with women finding significantly easier to get help than men.
Thus, overall, the study found that an important change had happened in this period. This was particularly the case regarding the option of having access to help at adopting technologies, which can be regarded as an important factor.
The studies are limited by a total response rate of 39% in 2019 and 45% in 2022. To compensate for this and reduce the impact of non-response bias, the data were weighed by gender, age, place of residence and education, so that it corresponds with the distribution in the population. The findings may, therefore, offer valuable information about the changes in adoption of new health information and communication technology among Icelanders´.
Conclusion
The purpose of the study was to understand better how the adoption of health information and communication technology has developed during the period 2019 to 2022. For policy implications, a better understanding of factors that relate to this can have implications for digital healthcare services and be used by health professionals and health authorities to work on improvements as needed.
There was a considerable increase in the use of the healthcare system for information tailored to people’s health and communication with health professionals. Furthermore, there was an important change in how people perceived their chances of adopting new technologies, with the possibilities being perceived to be much better in 2020 than in 2019. The outbreak of Covid-19 highlighted the importance of healthcare technology for information exchange between individuals and healthcare professionals. The period during which Covid-19 was active began in the early year of 2020, that is, after the first data collection took place, and was still ongoing when data for the second survey was collected. It is not possible to assert that the conditions during Covid-19, when it became more important for people to use technology for health information, caused a positive change in the perception of their possibilities to adopt health information and communication technology as well as their actual use of it. Nevertheless, it can be assumed that the Covid-19 situation, together with the fact that people had had more time to become knowledgeable about the healthcare system, were among the influencing factors. Thus, the results of the study indicate that people are likely to use health information and communication technology when the situation requires it, and they receive the necessary support to do so. It is, however, important to consider and support the needs of groups that are in a more vulnerable position, such as those who are getting older, so that they can have an equal opportunity to benefit from digital health. In addition, it is important that health authorities make an effort to introduce better the part of the healthcare system that offers reliable information from health professionals regarding various health related issues that are not directly connected to people’s health history.
About the author
Ágústa Pálsdóttir is a Professor in the Department of Information Science, School of Social Science, the University of Iceland. She received her bachelor’s degree in Library and Information Science and Master of Library and Information Science from the University of Iceland and PhD in Information Studies from the Department of Information Studies, Åbo Akademi University, Finland. She can be contacted at: agustap@hi.is
References
Ali, S.H., Foreman, J., Tozan, Y., Capasso, A., Jones, A.M. & DiClemente, R.J. (2020). Trends and predictors of COVID-19 information sources and their relationship with knowledge and beliefs related to the pandemic: nationwide cross-sectional study. JMIR Public Health Surveill, 6(4), e21071). https://doi.org/10.2196/21071
Alvarez, R.C. (2002). The promise of e-Health: a Canadian perspective. EHealth International, 1, 4. https://ehealthinternational.biomedcentral.com/articles/10.1186/1476-3591-1-4
Anderson, M. & Perrin, A. (2017). Tech adoption climbs among older adults: roughly two-thirds of those ages 65 and older go online and a record share now own smartphones: although many seniors remain relatively divorced from digital life. Pew Research Centre. https://www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults/
Arsad, F.S., Soffian, S.S.S., Kamaruddin, P.S.N.M., Nordin, N.R., Baharudin, M.H., Baharudin, U.M., Hassan, M.R., Nawi, A.M. & Ahmad, N. (2023). The impact of ehealth applications in healthcare intervention: a systematic review. Journal of Health Research, 37(3), 178-189. https://doi.org/10.56808/2586-940X.1020
Bhaskar, S., Bradley, S., Chattu, V.K., Adisesh, A., Nurtazina, A., Kyrykbayeva, S., Sakhamuri, S., Yaya, S., Sunil, T., Thomas, P., Mucci, V., Moguilner, S., Israel-Korn, S. Alacapa, J., Mishra, A., Pandya, S. Schroeder, S., Atreja, A., Banach, M. & Ray, D. (2020). Telemedicine, Covid 19, and disparities: Policy implications. Health Policy and Technology, 16(8), 556720. https://doi.org/10.3389/fpubh.2020.556720
Bidmon, S. & Terlutter, R. (2015). Gender differences in searching for health information on the internet and the virtual patient-physician relationship in Germany: exploratory results on how men and women differ and why. Journal of Medical Internet Research, 17(6), e156. https://doi.org/10.2196/jmir.4127
Bol, N., van Weert, J.C., Loos, E.F., Romano Bergstrom, J C., Bolle, S. & Smets, E.M. (2016). How are online health messages processed? using eye tracking to predict recall of information in younger and older adults. Journal of Health Communication, 21(4), 387-396. https://doi-org.zorac.aub.aau.dk/10.1080/10810730.2015.1080327
Budd, J., Miller, M.S., Manning, E.M., Lampos, V., Zhuang, M., Edelstein, M., Rees, G., Emery, V.C., Stevens, M.M., Keegan, N., Short, M.J., Pillay, D., Manley, E., Cox, I.J., Heymann, D., Johnson, A.M. & McKendry, R.A. (2020). Digital technologies in the public-health response to COVID-19. Nature Medicine, 26, 1183–1192. https://doi.org/10.1038/s41591-020-1011-4
Chong, A.Y.L., Blut, M. & Zheng, S. (2022). Factors influencing the acceptance of healthcare information technologies: A meta-analysis. Information & Management, 59(3), article 103604.
https://doi.org/10.1016/j.im.2022.103604
Crameri, K.-A., Maher, L. Van Dam, P. & Prior, S. (2022). Personal electronic healthcare records: What influences consumers to engage with their clinical data online? A literature review. Health Information Management Journal, 51(1), 3-12. https://doi.org/10.1177/1833358319895369
da Fonseca, M.H., Kovaleski, F., Picinin, C.T., Pedroso, B. & Rubbo, P. (2021). E-health practices and technologies: a systematic review from 2014 to 2019. https://doi.org/10.3390/healthcare9091192
Directory of Health: Heilsuvera: Mínar Heilbrigðisupplýsingar. (2016). https://www.landlaeknir.is/gaedi-og-eftirlit/heilbrigdisthjonusta/rafraen-sjukraskra/heilsuvera-minar-heilbrigdisupplysingar/
Dramé, D. (2020). The health crisis: fertile ground for disinformation. UNESCO Courier, 3, 24-26. https://en.unesco.org/courier/2020-3/health-crisis-fertile-ground-disinformation
Escoffery, C. (2018). Gender similarities and differences for e-health behaviors among U.S. adults. Telemedicine and e-Health, 24(5), 335-343. https://doi.org/10.1089/tmj.2017.0136
Eysenbach, G. (2001). What is e-health? Journal of Medical Internet Research, 3(2). https://doi.org/10.2196/jmir.3.2.e20
Gordon, N.P. & Crouch, E. (2019). Digital information technology use and patient preferences for internet-based health education modalities: cross-sectional survey study of middle-aged and older adults with chronic health conditions. JMIR Aging, 2(1), e12243. https://doi.org/10.2196/12243
Gu, D., Khan, S., Khan, I.U., Khan, S.U., Xie, Y., Li, X. & Zhan, G. (2021). Assessing the adoption of e-health technology in a developing country: an extension of the UTAUT Model. SAGE Open, 11(3). https://doi.org/10.1177/21582440211027565
Hallyburton A. & Evarts L.A. (2014). Gender and online health information seeking: a five survey meta-analysis. Journal of Consumer Health on the Internet, 18(2), 128-142. https://doi.org/10.1080/15398285.2014.902268
Health Records Act nr. 55 April 27, 2009. https://www.government.is/media/velferdarraduneyti-media/media/acrobat-enskar_sidur/Health-Records-Act-No-55-2009-as-amended-2016.pdf
Helsper, E.J. & Reisdorf, B.C. (2017). The emergence of a “digital underclass” in Great Britain and Sweden: changing reasons for digital exclusion. New Media & Society, 19(8), 1253–1270. https://doi.org/10.1177/1461444816634676
Holko, M., Litwin, T.R., Munoz, F., Theisz, K.I., Salgin, L., Jenks, N.P., Holmes, B.W., Watson-McGee, P., Winford, E. & Sharma, Y. (2022). Wearable fitness tracker use in federally qualified health center patients: strategies to improve the health of all of us using digital health devices. Digital Medicine, 5, 53. https://doi.org/10.1038/s41746-022-00593-x
Jatrana, S. & Crampton, P. (2009). Gender diferences in general practice utilisation
in New Zealand. Journal of Primary Health Care, 1, 261–9. https://doi.org/10.1071/HC09261
Jørgensen, J.T., Andersen, J.S., Tjønneland, A., Andersen, Z.J., Tjønneland, A. & Andersen, Z.J. Determinants related to gender diferences in general practice utilization: Danish diet, cancer and health cohort (2016). Scandinavian Journal of Primary Health Care, 34(3), 240-249. https://doi.org/10.1080/02813432.2016.1207141
Kontos, E., Blake, K.D., Chou, W.Y.S. & Prestin, A. (2012). Predictors of ehealth usage: insights on the digital divide from the health information national trends survey. Journal of Medical Internet Research, 16(7), e172 (2014). https://doi.org/10.2196/jmir.3117
Lindberg, B., Nilsson, C., Zotterman, D., Söderberg, S. & Skär, L. (2013). Using information and communication technology in home care for communication between patients, family members, and healthcare professionals: a systematic review. International Journal of Telemedicine and Applications, 461829. http://dx.doi.org/10.1155/2013/461829
Murphy, M., Scott, L.S., Salisbury, C., Turner, A., Scott, A., Denholm, R., Lewis, R., Iyer, G., Macleod, J. & Horwood, J. (2021). Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. British Journal of General Practice, 71(704). e167, (2021), https://doi.org/10.3399/BJGP.2020.0948
Ono, H. & Zavodny, M. (2007). Digital Inequality: a five-country comparison using microdata. Social Science Research, 36(3), 1135-1155.
Pálsdóttir, Á. (2012a). Elderly Icelanders and their relatives: Preferences for forms of information and problems experienced when seeking information. In: L. Hongxiu (Ed.), Studies on Inequalities in Information Society: Proceedings of the Conference, Well-Being in the Information Society, WIS 2012: August 22-24: TUCS Lecture Notes no 16, August 2012. Turku: Turku Centre for Computer Science.
Pálsdóttir, Á. (2012b). Relatives as supporters of elderly peoples´ information behaviour. Information Research, 17(4) paper 546. http://InformationR.net/ir/17-4/paper546.html
Sana, S., Kollmann, J., Magnée, T., Merkelbach, I., Denktaş, S. & Kocken, P.L. (2022). The role of socio-demographic and health factors during COVID-19 in remote access to GP care in low-income neighbourhoods: a cross-sectional survey of GP patients. BMC Primary Care, 23, 289. https://doi.org/10.1186/s12875-022-01887-5
Shao, M., Fan, J., Huang, Z. & Chen, M. (2022). The impact of information and communication technologies (ICTs) on health outcomes: a mediating effect analysis based on cross-national panel data. Journal of Environmental and Public Health, 2022, 2225723. https://doi.org/10.1155/2022/2225723
Singh, S., Evans, N., Williams, M., Sezginis, N. & Baryeh, N.A.K. (2018). Influences of socio-demographic factors and health utilization factors on patient-centered provider communication. Health Communication, 33(7), 917-23. https://doi.org/10.1080/10410236.2017.1322481
Statistics Iceland. (2014). Computer and internet usage in Iceland and other European countries 2013. Statistical Series: Tourism, Transport and IT, 99(1), 1-26. https://hagstofa.is/utgafur/utgafa/visindi-og-taekni/tolvu-og-netnotkun-a-islandi-og-i-odrum-evropulondum-2013/
Sun, R., Wu, L., Barnett, S., Deyo, P. & Swartwout, E. (2019). Socio-demographic predictors associated with capacity to engage in health care. Patient Experience Journal, 6(2), 35-41. https://doi.org/10.35680/2372-0247.1355
Tao, D., Wang, T., Wang, T., Zhang, T., Zhang, X. & Ku, X. (2020). A systematic review and meta-analysis of user acceptance of consumer-oriented health information technologies. Computers in Human Behavior, 104(2020), article 106147. https://doi.org/10.1016/j.chb.2019.09.023
Tapuria, A., Porat, T., Kalra, D., Dsouza, G., Xiaohui, S. & Curcin, V. (2021). Impact of patient access to their electronic health record: systematic review. Informatics for Health and Social Care, 46(2), 194-206. https://doi.org/10.1080/17538157.2021.1879810
Venkatesh, V., Morris, M. G., Davis, G. B., & Davis, F. D. (2003). Unified theory of acceptance and use of technology (UTAUT). MIS Quarterly, 27(3), 425-478. https://doi.org/10.1037/t57185-000
World Health Organization. (2020). Fighting misinformation in the time of CoVID-19, one click at the time. https://www.who.int/news-room/feature-stories/detail/fighting-misinformation-in-the-time-of-covid-19-one-click-at-a-time
World Health Organization. (2021). Global strategy on digital health 2020-2025. https://iris.who.int/bitstream/handle/10665/344249/9789240020924-eng.pdf