Effective factors influencing individual’s shared health decision making
Maedeh Ghorbanian Zolbin, Shengnan Han and Shahrokh Nikou
Introduction. This paper investigates the effects of information avoidance, information overload, health literacy on individuals’ shared health decision making.
Methods. A research model is proposed based on sound theoretical background. Data from 155 respondents was collected via an online survey.
Analysis. Partial Least Squares Structural Equation Modelling (PLS-SEM) was applied to analyse the data.
Results. The findings suggest that information overload and information avoidance both exhibit negative effects on an individual’s shared health decision making behaviour, while health literary possess positive effects. We also find that information avoidance has a positive impact on information avoidance. Moreover, health literacy is negatively related to both information overload and information avoidance.
Conclusions. The paper enhances both theoretical and empirical understanding of the effects of individuals’ health literacy, information overload and information avoidance on their shared health decision making behaviour. The results indicate that sufficient health literacy enables individuals to engage in their health decision making process and sharing their concerns with their physicians. However, information overload and information avoidance trigger negative effects which lead to individuals less involved in shared health decision making. Our results advocate more efforts to improve individual health literary as the means to mitigate the negative effects of information overload and information avoidance towards shared health decision making.
DOI: https://doi.org/10.47989/irisic2247
Introduction
Individuals' preferences for being included in the health decision-making process range from non-participation to full participation (Say, et al., 2006). Previous studies present three approaches. The first approach is for the physicians to take a dominant role and make decisions on behalf of patients (traditional paternalistic approaches) (Naik, et al., 2011). Thus, the role of patients is passive (Smith, et al., 2009). This is mainly because some people (e.g., older, less healthy, and less educated) prefer not to engage at all and defer all the decisions to the physician (Poon, et al., 2019). The second approach is called shared decision-making, referring to ‘the practical reconciliation of respect for persons (autonomy) and the monopoly and power of physicians’ (Godolphin, 2009, p. 2). In the process of shared decision making, the physicians are the experts on clinical evidence and individuals are the experts on what matters most to them (Bomhof-Roordink, et al., 2019; Poon, et al., 2019; Xiao, et al., 2021). The third approach is that individuals prefer to make independent medical decisions based on their own knowledge and understanding, without consultation with healthcare professionals (Seo, et al., 2016). Among the three approaches, the second approach, i.e. shared decision-making is increasingly advocated as the preferred model to engage individuals in the process of deciding about diagnosis, treatment, or follow-up when more than one medically reasonable option is available (Stiggelbout, et al., 2015). In other words, individuals’ involvement in the decision-making process has been more prioritized, and scholars have considered shared decision making as a significant element in patient-centred care (Steffensen, et al., 2018). This approach also resulted in various benefits for the individual patient (LeRouge et al., 2021; Zhai, et al., 2020). For example, increased satisfaction, reduced anxiety, better treatment adherence (Brabers, et al., 2017), increased health-related quality of life, reduced cost, and improved quality of personal care (Kehl, et al., 2015).
Individual shared health decision making behaviour is influenced by various factors, such as demographic variables (e.g. education, age, and gender), (Say, et al., 2006), the type of decisions that patients need to make, their experience of illness and medical care (Brabers, et al., 2017), self-efficacy (Negarandeh, et al., 2020), health literacy (Muscat, et al., 2020; Seo, et al., 2016), and how an individual deals with the information, which might be an enormous amount of information (information overload) (Liu and Kuo, 2016). Despite the relatively extensive literature on health literacy, information overload, and information avoidance (Heck and Meyer, 2019; Muscat, et al., 2019), there appears to be a paucity of research that explores and integrates these three determinants in the context of studying individuals’ share health decision-making behaviour.
In this paper, we aimed to study the effects of health literacy, information overload, and information avoidance on individual shared health decision making behaviour (Khaleel, et al., 2019). The rationale for conducting the study stems from the fact that with the proliferation of the Internet (re)sources individuals are facing abundant information to deal with (Beck, et al., 2014; Kim, 2020). When the volume and complexity of the available online information exceed individuals’ capacity to process the information, they face information overload (Eppler and Mengis, 2008), as people have a limited capacity to process and retain new information (Lee, et al., 2017). Consequently, the overload of information may lead to avoidance, ignoring or misinterpreting critical aspects of information, in the hope to lower stress, confusion, and cognitive strain (Lee, et al., 2017). As such, the availability of a large volume of online medical information could lead to information overload and information avoidance, subsequently impacting the share decision making adversely. Therefore, individuals may take decisions slowly with less quality, they may less prefer to participate in the health decision-making or even they may delegate all health decision-making responsibilities on healthcare professionals (Laker, et al., 2017). However, Jackson, et al., (2019) point out that health literacy is decisive in making individuals more informed, organised, and empowered to take control of the available health information, which can mitigate the deleterious effects of information overload. Thus, individuals are able to play an informed and active role in their health decision-makings (N’Goran, et al., 2018). Health literacy increases the capacity of individuals to obtain, interpret, and understand health information and enables them to be engaged in the medical decision making (Brabers, et al., 2017; Smith, et al., 2013). In addition, health literacy skills foster individuals’ ability to navigate complex healthcare systems, obtain appropriate health information (Goggins, et al., 2014; Poon, et al., 2019).
The paper enhances both theoretical and empirical understanding of the effects of individuals’ health literacy, information overload, and information avoidance on their shared health decision making behaviour. The results indicate that sufficient health literacy enables individuals to engage in their health decision making process and share their concerns with their physicians. However, information overload and information avoidance trigger negative effects which lead to individuals being less involved in shared health decision making. Our results advocate more efforts to improve individual health literacy as the means to mitigate the negative effects of information overload and information avoidance toward shared health decision making.
Theoretical background and hypothesis developments
Information overload and shared decision making
Information overload stands for ‘a perception on the part of the individual (or observations of that person) that the flow of information associated with work tasks is greater than can be managed effectively, in other words, a perception that overload in this sense creates a degree of stress for which his or her coping strategies are ineffective’ (Wilson, 2001, p. 113). Sweller (1988) considers information overload as ‘a state where the volume of the information exceeds an individual’s information processing capacity’ (Khaleel, et al., 2019, p. 1). Information overload depends on both complexity of the tasks and the decision-makers characteristics. First, the tasks with the characteristics of being complex, novel and knowledge-intensive can make individuals more susceptible to information overload. Second, decision makers with specific characteristics, such as less qualified, less educated, and less experienced, are more likely to face an overload of information (Eppler and Mengis, 2008). In general, information overload, or too much of information, affects individuals’ ability to process information accurately and efficiently (Laker, et al., 2017), and decreases their preference to actively participate in the context of medical decision making (Ghorbanian Zolbin, et al., 2021). Li and Chapman (2020) argue that selecting from an available large choice set of information is a difficult psychological task, sometimes leading to the decision maker violating normative principles such as dominance. Furthermore, Buchanan and Kock (2001) confirm that information overload is increasingly perceived as having an adverse effect on shared decision making because when people become overloaded, they cannot make decisions concerning what to ignore and what should garner their focus (Crook, et al., 2015). Therefore, we propose the following hypothesis:
H1: Information overload is negatively related to individual shared health decision making.
Information overload and information avoidance
While it is common perception that more information can produce better clarity, people are not always willing to acquire information, and on many occasions, they prefer to avoid information actively (e.g. by asking someone not to reveal information or by deciding not to read a text) (Karim, et al., 2019; Sweeny, et al., 2010). Information avoidance is defined as a behaviour that could either hamper or delay consumption of information, but more probably unwanted information (Fuertes, et al., 2019). Avoidance from information mostly happens when people prefer not to be active in the information-seeking process (Narayan, et al., 2011), and prefer to avoid potentially negative sensations (e.g. anxiety and stress), which is a potential way to counteract threats (Shu and Gino 2012). As Bawden and Robinson (2009) argued, too much information at hand, exacerbated by the multiple formats and channels available for its communication, can lead to information overload, which results in information avoidance (Fuertes, et al., 2019). Other studies (e.g., Chae, et al., 2019; Hong and Kim, 2020) also found that information overload could lead to information avoidance. Therefore, we propose:
H2: Information overload is positively related to information avoidance.
Health literacy and information overload
Health literacy refers to the extent to which ‘individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions for their own health matters’ (Kim, 2020, p. 22). Health literacy skills enable individuals to manage available health information, and it is directly linked with individuals’ ability and their motivation to handle information properly and effectively (Kim, et al., 2007), even if there are numerous amounts of complex information (Crook, et al., 2015). Therefore, there is an inverse association between health literacy and information overload (Jiang and Beaudoin, 2016). Individuals with higher levels of health literacy will perceive lower levels of information overload (Crook, et al., 2015). In other words, people with a lower level of health literacy capacity have a higher possibility of being overloaded by information, since the new and complex information is poorly understood or incorporated into existing knowledge. In addition, Hong and Kim (2020) found that low health literacy skills or lack of confidence in health information seeking express greater risk of information overload. Therefore, we propose:
H3: Health literacy is negatively related to information overload
Health literacy and information avoidance
While, on the one hand, some people prefer to be involved in the process of seeking and acquiring health information, on the other hand, some others, due to the special conditions (e.g. temporal and situational) prefer to avoid information. This preference could be a temporary solution to control their anxiety and stress to retain some hope (St Jean, et al., 2017). To have control over personal information-seeking behaviour and to reduce information avoidance behaviour among individuals, health literacy skills seem to be very significant factor. Since it enables people to understand and apply standard health messages (Strekalova, 2014). Scholars, such as Strekalova (2014) argued that there is a correlation between health literacy and information avoidance, and information avoidance is one of the results of low health literacy skills. In addition, Soroya, et al. (2021) and Orom, et al. (2018) confirmed the negative association between health literacy and health-related information avoidance behaviour. Therefore, we propose:
H4: Health literacy is negatively related to information avoidance.
Information avoidance and shared health decision making
Preference to be involved in the process of making medical decisions is highly dependent on the level of knowledge and understanding of the individuals. Therefore, individuals who attempts to avoid information actively or passively, cannot play a significant role in their health decision making (St Jean, et al., 2017). In a simple explanation, human being seeks information to make informed decisions, and they have possibilities of employing a variety of information (re)sources (e.g. media). For any reason, if individuals avoid obtaining or using existing information, they will fail in plying an active role in making decisions (Clark, 2005). Specially, in medical domains, avoiding information results in negative outcomes, such as high rate of morbidity, mortality, and higher healthcare expenditure (Heck and Meyer, 2019). Furthermore, individuals will be unable to fully participate in the health decision making process and they will shrink most of their health care responsibilities on physicians, and finally they will be less satisfied with the final health decisions (St Jean, et al., 2017). Other scholar (Clark, 2005; Degner, et al., 1997), also demonstrated the role of information avoidance in the preference of individual for participating in making medical decisions and indicated a correlation between these two variables. Therefore, we propose:
H5: Information avoidance is negatively related to individual shared health decision making.
Health literacy and shared health decision making
Individual’s preference to participate in health decisions is mostly shifting toward being more involved rather than just relying on healthcare professionals (Seo, et al., 2016). Shared decision making has come to the forefront as a way to improve health care for individuals by encouraging the production and dissemination of accurate, balanced, understandable health information and increasing individuals’ participation in shared health decision making (Lin and Fagerlin, 2014). Therefore, the initial step for being involved in the health decision making for individuals is being adequately informed and aware about their health condition and healthcare options (Gaglio, et al., 2012). In other words, to participate effectively and have a critical role in shared health decision making, people need to have the required skills, such as health literacy skills (Yin, et al., 2012), which enable them to be aware of where to look or ask for information, how to recognise, comprehend, and evaluate the credibility, validity, and trustworthiness of the information sources and finally how to use the information to actively participate in the shared medical decision making (Gaglio, et al., 2012). Politi, et al. (2013) argued that higher health literacy empowers individuals to participate in decision making, as well as to support physicians in engaging with individual. Furthermore, scholars (e.g. Goggins, et al., 2014; Roh, et al., 2018) acknowledged that people with higher levels of health literacy desire more participation and more involvement in the problem-solving and shared decision making process than people with low health literacy. Therefore, we propose:
H6: Health literacy is positively related to individual shared health decision making
Based on the theoretical understandings and the proposed hypothesis, the research model is illustrated in Figure 1.
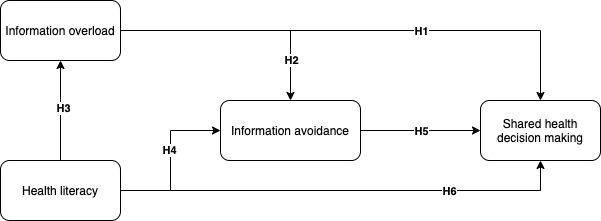
Figure 1: Research model
Research methods
Instrument and data collection
In order to collect quantitative date, we designed a questionnaire including demographic information and four different sets of statements (health literacy, information overload, information avoidance and shared health decision making) for measuring the constructs. All items for measuring constructs were derived from previously validated measures, and if needed, some changes were made to fit the study context. Twelve items derived from studies by Zhang, et al. (2016) and Maier, et al. (2015) considered to measure information overload. Seven items for measuring information avoidance were obtained from Shin and Lin (2016). In addition, seven items for measuring health literacy were derived from studies by Chinn and McCarthy (2013) and Nutbeam (2000). Finally, five items for measuring individual health decision making preferences were derived from the study by Seo, et al. (2016). The aim of this survey is to collect data to test the hypothesis and verify the suggested model. The online survey is based on the Likert scale (from completely agree to completely disagree). We sent out more than 230 online survey invitations in 2021, using different channels such as university mailing lists, authors’ personal networks, and social media platforms. In total, we received 172 responses, where 155 were complete responses.
Descriptive and measurement results
The respondents’ age was: 18–25 years (n = 19, 12.3%), 26–35 years (n = 74, 47.7%), 36–45 years (n = 32, 20.6%), 46–55 years (n = 28, 18.1%), and over 55 years (n = 2, 1.3%). The sample includes 78 females, 67 males, besides 10 participants preferred not to reveal their gender. The educational level of the respondents was as follows: high school diploma (n = 6), bachelor’s degree (n = 32), master’s degree (n = 85), and PhD degree (n = 29), and 3 indicated other educational attainments. Regarding to the current occupational status, most of the participants were students (n = 69), 54 were self-employed, 13 were non-employed, 12 were employed, and only 7 of the participants held some other occupation. In the sample, there were 64 Finnish and 91 non-Finnish respondents.
The internal reliability of the data was assessed through several statistical test, such as items loadings, Cronbach Alpha, Composite Reliability (CR), and Average Variance Extracted (AVE), following the Hair, et al.’s (2019), recommendation. Expect for few items, all other items within their respective constructs were loaded above the recommended threshold of 0.70. Moreover, the Alpha value for all constructs was above cut-off value, the lowest was (0.89), for information avoidance, and the highest was (0.91), for information overload. All constructs had acceptable CR value, the lowest was for information avoidance (0.89) and the highest was for shared health decision making (0.93). Finally, the AVE values for all constructs were above the recommended value of 0.50, ranging from 0.59 (information avoidance) to 0.75 (health decision making). We also examined the constructs’ discriminate validity using the Fornell Larcker criterion (Fornell and Larcker, 1981) by accounting for the AVE scores, and all AVE values were lower than the shared variance for all model constructs. The results support the discriminant validity (Table 1).
| HLIT | IAOI | IOVE | SHDM | |
|---|---|---|---|---|
| Health literacy | 0.635 | |||
| Information avoidance | -0.319 | 0.667 | Information overload | -0.264 | 0.207 | 0.832 | Shared health decision making | 0.126 | -0.209 | -0.170 | 0.840 |
Structural Models
The PLS-SEM (partial least squares structural equation modelling) was used to investigate path relationships proposed in the research model. The structural results showed that the independent variable (shared health decision making) was explained by variance of 29%. The two predictors (information overload, and information avoidance) were explained by variance of 16% and 12%, respectively. The SEM results showed that information overload is negatively related to shared decision-making (β = -0.21; t = 3.341; p = 0.001); therefore, H1 was supported by the model. Moreover, the SEM results showed that information overload was positively related to information avoidance (β = 0.17; t = 2.745; p = 0.005), thus, H2 was also supported. In addition, the SEM results supported both H3 and H4, where we hypothesised that health literacy is negatively related to information overload (β = -0.37; t = 6.189; p = 0.001), and negatively related to information avoidance (β = -0.12; t = 3.126; p = 0.05). The SEM results showed that there is a negative association between information avoidance and shared health decision making (β = -0.28; t = 6.783 p = 0.001); thus, H5 was supported by the model.
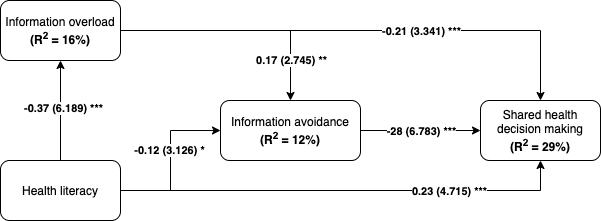
Figure 2: Research model test results
Discussion and conclusion
In this paper, we have empirically examined the effects of health literacy, information overload and information avoidance on individual shared health decision making. To meet this purpose, we distributed 230 online surveys among different groups of people, living in Finland, and finally we received 155 useful responses. The results support the hypotheses (H1 and H5) that information overload and information avoidance both exhibit negative effects on individual’s shared health decision making behaviour, while health literary possesses positive effects (H6). We recognise that a patient’s level of preference to participate in share health decision-making depends on their health literacy, especially when they are overloaded with a massive amount of information.
Results of the study indicate that less preference to participate in the health share decision making process occurs when individuals, who need to participate in decision making, face a massive amount of information that is more than their information processing capacity i.e., or they face a multitude of resource(s) which confuse them in case of trusting and selecting one specific source. This situation, in most cases, leads to ignoring and avoiding the information to release from overthinking and overprocessing. Therefore, individuals prefer to avoid participating in health decision making and delegate decision making responsibility to the health care professionals, since individuals do not have enough knowledge to exchange. On the other hand, this study expresses that health literacy is a significant determinant factor affecting individuals’ shared health decision making preferences and empowers them to actively participate and share their opinion with healthcare professionals, even though they are overloaded with a massive amount of health information through different channels. In other words, health literacy empowers individuals to acquire reliable and trustworthy information, especially when there are risks of avoiding and ignoring information due to the high availability and accessibility and applying that information in their shared health decision making process. The result of this study is highly appreciated by individuals, who are at risk of more health issues, and by healthcare professionals in case of reducing their responsibilities. Furthermore, from the societal aspect, risk of health and social inequalities will decrease when large community can make shared health decisions, particularly if those sectors represent some of the least healthy, least knowledgeable, and least engaged patients.
The results of this study are in line with previous studies. For example, our study indicates that information overload by itself has a negative effect on share health decision making (H1). Other studies, such as Buchanan and Kock (2001) and Crook, et al. (2015) prove the adverse relationship between information overload and shared health decision making; more available information leads to less preference to take part in heath share decision making. Furthermore, information overload would increase individuals’ behaviour of information avoidance (H2) when acquiring health information, which results in their less involvement in shared health decision making (H5). This finding is approved by Bawden and Robinson (2009) and Clark (2005). They state that information overload can lead to information avoidance, and consequently impact an individual’s health decision making choices. In other words, when information exceeds the receiver’s ability to process, the receivers often prefer to ignore or avoid the information and defer all the health decisions to healthcare professionals (Lee, et al., 2017). In addition, study by Bettis-Outland (2012) stressed that information avoidance is one of the negative outcomes of the availability of massive amount of health-related information, this means that individuals would prefer to leave all decisions about their health issues to their doctors or healthcare professionals and avoid patient-doctor information exchange (Poon, et al., 2019). In addition, an overload of information is a hindrance rather than a help for people who are facing it (Bawden, et al., 1999), specifically for those who lack sufficient literacy skills (Jiang and Beaudoin, 2016). Therefore, it is not unusual when information overload occurs, people tend to avoid it completely. This avoidance may result in less knowledge and understanding of critical issues, such as health issues, which affects individuals’ tendency to participate in their medical decision-making. In other words, individuals with less knowledge may have to leave all their decision-making responsibilities to their physician.
Additionally, our results support the hypotheses that individual health literacy have negative effects on individual’s behaviour towards information overload (H3) and information avoidance (H4). When people are faced with a large amount of health-related information, their ability to distinguish the trusted and reliable information (re)sources and their capacity for gathering, processing, and understanding health-related information is highly valued. Prior studies support this argument. For example, Hong and Kim (2020) indicate that people who have a lower health literacy or a confidence in health information seeking express greater information overload behaviour. Scholars, such as Crook, et al. (2015) and Strekalova (2014) investigated the relation between health literacy and information overload and information avoidance as well. In both studies higher health literacy leads to lower information overload and information avoidance. Furthermore, our study highlighted the importance of health literacy in shared health decision making (H6). The result indicates a positive effect of health literacy on shared health decision making. Other researchers such as DeWalt, et al. (2007) have also found that individuals with lower health literacy, experience worse patient-doctor information exchange. In addition, Ishikawa, et al. (2009) indicated that individuals who have higher health literacy have more desire to participate in medical decision-making. Therefore, due to the positive and direct impact of health literacy on individuals’ shared health decision making, we advocate more efforts to improve individual health literacy as the means to mitigate the negative effects of information overload and information avoidance towards shared health decision making.
Limitations and future work
This paper has some limitations. First, our results are based on limited sample size. Therefore, we cannot claim that the results are generalisable. Second, this study investigates the relationships between information overload, information avoidance, health literacy, and shared decision making in general without considering any specific context or a health problem. In the future, scholars can consider the proposed model in a particular health decision context, such as cancer. In addition, this study does not consider personal characteristics (e.g. age or education) in its analysis. Thereby, future investigations can consider these variables and perform multi-group analysis to see if any differences or similarities can be found based on the gender or the age of individuals.
About the authors
Maedeh Ghorbanian Zolbin is a doctoral candidate at the Faculty of Social Science, Business and Economic, Åbo Akademi University. She obtained her master’s degree in Business Administration-International Marketing at Zanjan University, Iran in 2016. Her research focuses on health literacy, digital health service usage, Elderly people, Elderly immigrants, health decision making, and health tourism. Maedeh Ghorbanian Zolbin can be contacted at maedeh.ghorbanianzolbin@abo.fi.
Shengnan Han is an associate professor at the Department of Computer and Systems Sciences, Stockholm University, Sweden. She obtained her D.Sc. (Economics) in information systems at Åbo Akademi University, Finland in 2005. Her research focuses on digital transformation (AI & digital innovations), sustainability, business processes management, and user acceptance of technology. Shengman Han can be contacted at shengnan@dsv.su.se.
Shahrokh Nikou is a Senior Lecturer at the Faculty of Social Sciences, Business and Economics, Åbo Akademi University. He received a doctorate from ÅAU in 2012 and became a Docent in Information Systems in 2014. He has a MSc in Computer Networks from the Royal University of Technology, Stockholm (Sweden), 2008, and an MSc in Computer Sciences from ÅAU 2009. His research interests relate to digitalisation in entrepreneurship, healthcare services and higher education with a particular focus on digital transformation as enablers for organisational change. Shahrokh Nikou can be contacted at shahrokh.nikou@abo.fi.
References
- Bawden, D., Holtham, C., & Courtney, N. (1999). Perspectives on information overload. Aslib proceedings. 51(8), 249-155. PMID: https://doi.org/10.1108/EUM0000000006984
- Bawden, D., & Robinson, L. (2009). The dark side of information: overload, anxiety and other paradoxes and pathologies. Journal of Information Science, 35(2), 180-191. https://doi.org/10.1177/0165551508095781
- Beck, F., Richard, J. B., Nguyen-Thanh, V., Montagni, I., Parizot, I., & Renahy, E. (2014). Use of the Internet as a Health Information Resource Among French Young Adults: Results from a Nationally Representative Survey. Journal of Medical Internet Research, 16,(5), 1-13. https://doi.org/10.2196/jmir.2934
- Bomhof-Roordink, H., Gärtner, F. R., Stiggelbout, A. M., & Pieterse, A. H. (2019). Key components of shared decision-making models: a systematic review. BMJ Open, 9(12), e031763. https://doi.org/10.1136/bmjopen-2019-031763
- Brabers, A. E. M., Rademakers, J. J. D. J. M., Groenewegen, P. P., van Dijk, L., & de Jong, J. D. (2017). What role does health literacy play in patients’ involvement in medical decision-making? PLoS ONE, 12 (3), e0173316. https://doi.org/10.1371/journal.pone.0173316
- Buchanan, J., & Kock, N. (2001). Information Overload: A Decision-Making Perspective. Multiple Criteria Decision Making in the New Millennium. , 49–58. https://doi.org/10.1007/978-3-642-56680-6_4
- Chae, J., Lee, C.-J., & Kim, K. (2019). Prevalence, Predictors, and Psychosocial Mechanism of Cancer Information Avoidance: Findings from a National Survey of U.S. Adults. Health Communication , 1-9. https://doi.org/10.1080/10410236.2018.1563028
- Chinn, D., & McCarthy, C. (2013). All Aspects of Health Literacy Scale (AAHLS): developing a tool to measure functional, communicative, and critical health literacy in primary healthcare settings. Patient Education and Counselling, 90(2), 247-253. https://doi.org/10.1016/j.pec.2012.10.019
- Clark, J. (2005). Constructing expertise: Inequality and the consequences of information-seeking by breast cancer patients. Illness, Crisis & Loss, 13(2), 169-185. https://doi.org/10.1177/105413730501300207
- Crook, B., Stephens, K. K., Pastorek, A. E., Mackert, M., & Donovan, E. E. (2015). Sharing health information and influencing behavioral intentions: The role of health literacy, information overload, and the Internet in the diffusion of healthy heart information. Health Communication, 31, 60-71. https://doi.org/10.1080/10410236.2014.936336
- Degner, L. F., Kristjanson, L. J., Bowman, D., Sloan, J. A., Carriere, K. C., O'Neil, J., Bilodeau, B., Watson, P., & Mueller, B. (1997). Information needs and decisional preferences in women with breast cancer. JAMA, 27718, 1485-1492. PMID: 9145723
- DeWalt, D. A., Boone, R. S., & Pignone, M. P. (2007). Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. American Journal of Health Behaviour, 31(1), S27-S35. https://doi.org/10.5555/ajhb.2007.31.supp.S27
- Eppler, M. J., & Mengis, J. (2008). The concept of information overload-a review of literature from organization science, accounting, marketing, mis, and related disciplines (2004). Kommunikationsmanagement im Wandel. , 271-305. https://doi.org/10.1007/978-3-8349-9772-2_15
- Fornell, C. G., & Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research 18(1), 39–50. https://doi.org/10.2307/3151312
- Fuertes, M. C. M., Jose, B. M. D., Nem Singh, M. A. A., Rubio, P. E. P., & de Guzman, A. B. (2019). The moderating effects of information overload and academic procrastination on the information avoidance behaviour among Filipino undergraduate thesis writers. Journal of Librarianship and Information Science, 52(3), 694-712. https://doi.org/10.1177/0961000619871608
- Gaglio, B., Glasgow, R. E., & Bull, S. S. (2012). Do patient preferences for health information vary by health literacy or numeracy? A qualitative assessment. Journal of Health Communication, 17(sup3), 109-121. https://doi.org/10.1080/10810730.2012.712616
- Ghorbanian Zolbin, M., Kainat, K., & Nikou, S. (2021). Health Information Literacy: The Saving Grace During Traumatic Times. Bled e-conference. , 294-308. https://doi.org/10.18690/978-961-286-385-9.22
- Godolphin, W. (2009). Shared Decision-Making. Healthcare Quarterly, 12(sp), e186–e190. https://doi.org/10.12927/hcq.2009.20947
- Goggins, K. M., Wallston, K. A., Nwosu, S., Schildcrout, J. S., Castel, L., & Kripalani, S. (2014). Health literacy, numeracy, and other characteristics associated with hospitalized patients' preferences for involvement in decision making. Journal of Health Communication, 19(sup2), 29-43. https://doi.org/10.1080/10810730.2014.938841
- Hair, J. F., Risher, J. J., Sarstedt, M., & Ringle. C. M. (2019). When to use and how to report the results of PLS-SEM. European Business Review, 31(1), 2-24.https://doi.org/10.1108/EBR-11-2018-0203
- Heck, P. R., & Meyer, M. N. (2019). Information Avoidance in Genetic Health: Perceptions, Norms, and Preferences. JSocial Cognition, 37(3), 266–293. https://doi.org/10.1521/soco.2019.37.3.266
- Hong, H., & Kim, H. J. (2020). Antecedents and Consequences of Information Overload in the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 17(24), 9305. https://doi.org/10.3390/ijerph17249305
- Ishikawa, H., Yano, E., Fujimori, S., Kinoshita, M., Yamanouchi, T., Yoshikawa, M., Yamazaki, Y., & Teramoto, T. (2009). Patient health literacy and patient–physician information exchange during a visit.Patient health literacy and patient–physician information exchange during a visit. Family Practice, 26(6), 517-523. https://doi.org/10.1093/fampra/cmp060
- Jackson, Y., Janssen, E., Fischer, R., Beaverson, K., Loftus, J., Betteridge, K., Rhoten, S., Flood, E., & Lundie, M. (2019). The evolving role of patient preference studies in health-care decision-making, from clinical drug development to clinical care management. Expert Review of Pharmacoeconomics & Outcomes Research, 19(4), 383–396. https://doi.org/10.1080/14737167.2019.1612242
- Jiang, S., & Beaudoin, C. E. (2016). Health literacy and the internet: An exploratory study on the 2013 HINTS survey. Computers in Human Behaviour, 58, 240–248. https://doi.org/10.1016/j.chb.2016.01.007
- Karim, M., Widén, G., & Heinström, J. (2019). Influence of demographics and information literacy self-efficacy on information avoidance propensity among youth. In Proceedings of CoLIS, the Tenth International Conference on Conceptions of Library and Information Science. Information Research, 24(4). http://InformationR.net/ir/24-4/colis/colis1909.html (Internet Archive)
- Kehl, K. L., Landrum, M. B., Arora, N. K., Ganz, P. A., van Ryn, M., Mack, J. W., & Keating, N. L. (2015). Association of Actual and Preferred Decision Roles with Patient-Reported Quality of Care. JAMA Oncology, 1(1), 50.https://doi.org/10.1001/jamaoncol.2014.112
- Khaleel, I., Wimmer, B. C., Peterson, G. M., Zaidi, S. T. R., Roehrer, E., Cummings, E., & Lee, K. (2019). Health information overload among health consumers: a scoping review. APatient Education and Counselling, 103(1), 15-32. https://doi.org/10.1016/j.pec.2019.08.008
- Kim, K., Lustria, M. L. A., Burke, D., & Kwon, N. (2007). Predictors of cancer information overload: findings from a national survey. Information Research, 12(4), 12-4. http://InformationR.net/ir/12-4/paper326.html (Internet Archive)
- Kim, S. (2020). Caregivers’ Information Overload and Their Personal Health Literacy. IWestern Journal of Nursing Research, 43(5), 431–441.https://doi.org/10.1177/0193945920959086
- Laker, L. F., Froehle, C. M., Windeler, J. B., & Lindsell, C. J. (2017). Quality and Efficiency of the Clinical Decision-Making Process: Information Overload and Emphasis Framing. Production and Operations Management, 27(12), 2213-2225. https://doi.org/10.1111/poms.12777
- Lee, K., Roehrer, E., & Cummings, E. (2017). Information overload in consumers of health-related information: a scoping review protocol. JBI Evidence Synthesis, 15(10), 2457-2463.https://doi.org/10.11124/JBISRIR-2016-003287
- LeRouge, C., Nguyen, A. M., & Bowen, D. J. (2021). Patient Decision Aid Selection for Shared Decision Making: A Multicase Qualitative Study. Medical Care Research and Review, 79(2). https://doi.org/10.1177/10775587211012995
- Lin, G. A., & Fagerlin, A. (2014). Shared decision-making state of the science. Circulation: Cardiovascular Quality and Outcomes, 7(2), 328-334.https://doi.org/10.1161/CIRCOUTCOMES.113.000322
- Liu, C.-F., & Kuo, K.-M. (2016). Does information overload prevent chronic patients from reading self-management educational materials? International Journal of Medical Informatics, 89, 1–8.https://doi.org/10.1016/j.ijmedinf.2016.01.01
- Maier, C., Laumer, S., Eckhardt, A., & Weitzel, T. (2015). Giving too much social support: social overload on social networking sites. European Journal of Information Systems, 24(5), 447-464. https://doi.org/10.1057/ejis.2014.3
- Muscat, D. M., Morony, S., Trevena, L., Hayen, A., Shepherd, H. L., Smith, S. K., Dhillon, H. M., Luxford, K., Nutbeam, D., & McCaffery, K. J. (2019). Skills for Shared Decision-Making: Evaluation of a Health Literacy Program for Consumers with Lower Literacy Levels. Health Literacy Research and Practice, 3(3), 558-574. https://doi.org/10.3928/24748307-20190408-02
- Muscat, D. M., Shepherd, H. L., Nutbeam, D., Trevena, L., & McCaffery, K. J. (2020). Health Literacy and Shared Decision-making: Exploring the Relationship to Enable Meaningful Patient Engagement in Healthcare. Journal of General Internal Medicine, 36(2), 521-524. https://doi.org/10.1007/s11606-020-05912-0
- N’Goran, A. A., Pasquier, J., Deruaz-Luyet, A., Burnand, B., Haller, D. M., Neuner-Jehle, S., & Bodenmann, P. (2018). Factors associated with health literacy in multimorbid patients in primary care: a cross-sectional study in Switzerland. BMJ Open, 8(2), e018281. https://doi.org/10.1136/bmjopen-2017-018281
- Naik, A. D., Street Jr, R. L., Castillo, D., & Abraham, N. S. (2011). Health literacy and decision-making styles for complex antithrombotic therapy among older multimorbid adults. atient Education and Counselling, 85(3), 499-504.https://doi.org/10.1016/j.pec.2010.12.015
- Narayan, B., Case, D. O., & Edwards, S. L. (2011). The role of information avoidance in everyday-life information behaviours. Proceedings of the American Society for Information Science and Technology, 48(1) 1-7.https://doi.org/10.1002/meet.2011.14504801085
- Negarandeh, R., Yazdani, Z., Lehto, R., & Lashkari, M. (2020). The Effect of Using the Question Prompt List on Shared Decision Making, Self-Efficacy in Decision Making, and Preferences for Participation Among Women with Breast Cancer: A Study Protocol. International Journal of Cancer Management. 13 (8). https://doi.org/10.5812/ijcm.103873
- Nutbeam, D. (2000). Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15(3), 259-267. https://doi.org/10.1093/heapro/15.3.259
- Orom, H., Schofield, E., Kiviniemi, M. T., Waters, E. A., Biddle, C., Chen, X., Li, Y., Kaphingst, K. A., & Hay, J. L. (2018). Low Health Literacy and Health Information Avoidance but Not Satisficing Help Explain “Don’t Know” Responses to Questions Assessing Perceived Risk. Medical Decision Making, 38(112), 1006–1017. https://doi.org/10.1177/0272989X18799999
- Politi, M. C., Dizon, D. S., Frosch, D. L., Kuzemchak, M. D., & Stiggelbout, A. M. (2013). Importance of clarifying patients’ desired role in shared decision making to match their level of engagement with their preferences. Bmj, 347(5), 1-12. https://doi.org/10.1136/bmj.f7066
- Poon, B. Y., Shortell, S. M., & Rodriguez, H. P. (2019). Patient Activation as a Pathway to Shared Decision-making for Adults with Diabetes or Cardiovascular Disease. Journal of General Internal Medicine. 35(3), 732-742. https://doi.org/10.1007/s11606-019-05351-6
- Roh, Y. H., Do Koh, Y., Kim, J. O., Noh, J. H., Gong, H. S., & Baek, G. H. (2018). Patients with limited health literacy have similar preferences but different perceptions in surgical decision-making for carpal tunnel release. Clinical Orthopaedics and Related Research, 476(4), 846. https://doi.org/10.1007/s11999.0000000000000075
- Say, R., Murtagh, M., & Thomson, R. (2006). Patients’ preference for involvement in medical decision making: A narrative review. Patient Education and Counselling, 60(2), 102–114. https://doi.org/10.1016/j.pec.2005.02.003
- Seo, J., Goodman, M. S., Politi, M., Blanchard, M., & Kaphingst, K. A. (2016). Effect of Health Literacy on Decision-Making Preferences among Medically Underserved Patients. Medical Decision Making, 36(4), 550–556. https://doi.org/10.1177/0272989X16632197
- Shin, W., & Lin, T. T. C. (2016). Who avoids location-based advertising and why? Investigating the relationship between user perceptions and advertising avoidance. Computers in Human Behaviour, 63, 444-452. https://doi.org/10.1016/j.chb.2016.05.036
- Shu, L. L., & Gino, F. (2012). Sweeping dishonesty under the rug: How unethical actions lead to forgetting of moral rules. Journal of Personality and Social Psychology, 102(6), 1164-1177. https://doi.org/10.1037/a0028381
- Smith, S. K., Dixon, A., Trevena, L., Nutbeam, D., & McCaffery, K. J. (2009). Exploring patient involvement in healthcare decision making across different education and functional health literacy groups.Social Science & Medicine, 69(12), 1805–1812. https://doi.org/10.1016/j.socscimed.2009.09.056
- Smith, S. K., Nutbeam, D., & McCaffery, K. J. (2013). Insights into the concept and measurement of health literacy from a study of shared decision-making in a low literacy population.Journal of Health Psychology, 18(8), 1011–1022. https://doi.org/10.1177/1359105312468192
- Soroya, S. H., Farooq, A., Mahmood, K., Isoaho, J., & Zara, S. (2021). From information seeking to information avoidance: Understanding the health information behaviour during a global health crisis.Information Processing & Management, 58(2), 102440. https://doi.org/10.1016/j.ipm.2020.102440
- St Jean, B., Jindal, G., & Liao, Y. (2017). Is ignorance really bliss? Exploring the interrelationships among information avoidance, health literacy and health justice. Proceedings of the Association for Information Science and Technology, 54(1), 394–404. https://doi.org/10.1002/pra2.2017.14505401043
- Steffensen, K. D., Vinter, M., Crüger, D., Dankl, K., Coulter, A., Stuart, B., & Berry, L. L. (2018). Lessons in Integrating Shared Decision-Making into Cancer Care. Journal of Oncology Practice, 14(4), 229–235. https://doi.org/10.1200/JOP.18.00019
- Stiggelbout, A. M., Pieterse, A. H., & De Haes, J. C. J. M. (2015). Shared decision making: Concepts, evidence, and practice. Patient Education and Counseling, 98(10), 1172–1179. https://doi.org/10.1016/j.pec.2015.06.022
- Strekalova, Y. A. (2014). Seekers and avoiders: using health information orientation to explore audience segmentation. Journal of Communication in Healthcare, 7(3), 228-237. https://doi.org/10.1179/1753807614Y.0000000058
- Sweeny, K., Melnyk, D., Miller, W., & Shepperd. J. (2010). Information avoidance: Who, what, when, and why. Review of General Psychology, 14(4), 340-353. https://doi.org/10.1037/a0021288
- Sweller, J. (1988). Cognitive load during problem solving: effects on learning. Cognitive Science, 12(2), 257–285. https://doi.org/10.1016/0364-0213(88)90023-7
- Wilson, T. D. (2001). Information overload: implications for healthcare services. Health Informatics Journal, 7, 112-117. https://doi.org/10.1177/146045820100700210
- Xiao, L., Miao, J., Peng, M., Jiang, H., Liu, S., Liu, Y., & Zhang, L. (2021). The effect of health literacy on patient’s perceived shared decision‐making among Chinese cancer patients. Psycho-Oncology, 31(1), 70-77. https://doi.org/10.1002/pon.5777
- Yin, H. S. Dreyer, B. P., Vivar, K. L., MacFarland, S., Van Schaick, L., & Mendelsohn, A. L. (2012). Perceived barriers to care and attitudes towards shared decision-making among low socioeconomic status parents: Role of health literacy. Academic Pediatrics, 12, 117– 24.https://doi.org/10.1016/j.acap.2012.01.001
- Zhai, H., Lavender, C., Li, C., Wu, H., Gong, N., & Cheng, Y. (2020). Who decides? Shared decision-making among colorectal cancer surgery patients in China. Supportive Care in Cancer, 28(11), 5353-5361.https://doi.org/10.1007/s00520-020-05391-3
- Zhang, S., Zhao, L., Lu, Y., & Yang, J. (2016). Do you get tired of socializing? An empirical explanation of discontinuous usage behaviour in social network services. Information & Management, 53(7), 904-914.https://doi.org/10.1016/j.im.2016.03.006